
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
FISCAL YEAR 2018
AUDITED FINANCIAL STATEMENTS
Table of Contents
Agency Head Message ..................................................................................... 1
Management’s Discussion and Analysis .......................................................... 2
Principal Statements ....................................................................................... 20
Notes to the Principal Statements ................................................................... 25
Other Information ........................................................................................... 41
Independent Auditor’s Reports ....................................................................... 59

1
Agency Head Message
The Military Health System (MHS) serves as the Department of
Defense’s singular health care delivery entity responsible and
accountable for effectively and efficiently maintaining and advancing
our dual missions of readiness and health-care delivery for our 9.5
million service member, retiree, and family member beneficiaries.
The MHS prides itself on its commitment to service and its corporate
culture which includes a strong obligation to transparency, especially
as we plan for a more integrated, higher-performing enterprise in light
of our significant Congressionally mandated transitions required by
the 2017 and 2019 National Defense Authorization Acts. The mission
of the MHS remains to support the warfighter, care for our warfighter
families and care for our patient. As in the past, our priority remains
readiness in support of the warfighting mission of the Department of
Defense, and we provide that through our high quality health care
system. The ultimate goal of this transition is a more integrated,
efficient and effective system of readiness and health that best
supports the lethality of the force. In order to achieve that lofty goal,
the MHS must ensure proper controls are in place, that they are
functioning as intended, and that we are maximizing our value to our
beneficiaries and to the Department.
The ongoing auditability of the MHS is a priority for each and every member of our team as each of us directly
contributes to our mission, regardless of rank or level, and the entire enterprise is committed to achieving an unmodified
opinion. We understand it will take everyone’s support to improve the reliability and accuracy of our data to enable us
to make informed decisions both now and in the future and make the best use of our available resources in order to
achieve our strategic goals and objectives. In order to continue our progress towards this goal, we have undertaken
corrective actions based on deficiencies and internal control weaknesses that our team has identified. More information
regarding the status of the internal control environment within the DHP Enterprise and the steps we are taking to
address these issues can be found in the Management Assurance section of this report.
I welcome and encourage all of our stakeholders to read this report. I am confident that in doing so, it will be clear that
the MHS is committed to transparency, efficiency, and effectiveness as we ensure mission alignment with Secretary
Mattis’ Department priorities to increase lethality, leverage strategic partnerships, and improve our business processes. I
thank the staff of the MHS for their tireless dedication and perseverance in delivering these strategic priorities every
day, our beneficiaries for their service and being the most deserving customers in the world, and all our stakeholders for
their incredible support as we engage in this endeavor.
Tom McCaffery
Principle Deputy Assistant Secretary of Defense for Health Affairs
2
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
MANAGEMENT’S DISCUSSION AND
ANALYSIS

Management’s Discussion and Analysis
3
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
MANAGEMENT’S DISCUSSION AND ANALYSIS
YEARS ENDED SEPTEMBER 30, 2018 AND 2017
I Description of the Reporting Entity
The reporting entity is the Contract Resource Management (CRM) division of the Defense Health Agency (DHA) of
the Department of Defense (DoD). Within DoD, the Office of the Under Secretary of Defense (OUSD) for
Personnel and Readiness (P&R), through the Office of the Assistant Secretary of Defense (OASD) for Health Affairs
(HA), has as one of its missions, operational oversight of the Military Health System (MHS), including the direct
care system (military hospitals), the private sector care system, and the Medicare-Eligible Retiree Health Care Fund
(MERHCF) for those beneficiaries dual-eligible for both Medicare and TRICARE. The Defense Finance and
Accounting Service-Indianapolis (DFAS-IN) provides accounting and financing activities for DHA.
The primary mission of the DHA, a Combat Support Agency, is to enhance the DoD and our nation’s security by
providing health care support for the full range of military operations and sustaining the health of all those entrusted
to our care, including active duty personnel, military retirees, certain members of the Reserve Component, family
members, widows, survivors, ex-spouses, and other eligible members. These beneficiaries receive direct care
through Military Treatment Facilities (MTFs), private sector care through TRICARE's civilian provider network,
prescription and mail order coverage through the TRICARE Pharmacy Program (TPHARM). Care is also provided
to members of the Coast Guard, the National Oceanic and Atmospheric Administration (NOAA), the Public Health
Service (PHS) and their families on a reimbursable basis.
The DHA supports the delivery of integrated, affordable, and high quality health services to beneficiaries of the
MHS, and executes responsibility for shared services, functions and activities of the MHS and other common clinical
and business processes in support of the Military Services. The DHA serves as the program manager of the
TRICARE health plan, medical resources, and the market manager for the National Capital Region (NCR) enhanced
Multi-Service Market. The DHA manages the execution of policy as issued by the OASD(HA) and exercises
authority, direction, and control over the inpatient facilities and their subordinate clinics assigned to the DHA in the
NCR Directorate.
The senior medical leadership, the Surgeons General, and DHA staff over the past several years have reexamined
DHA’s fundamental purpose, vision for the future and strategies to achieve that vision. The DHA is refocusing
efforts on the core business in which it is engaged: creating an integrated medical team that provides optimal health
services in support of our nation’s military mission—anytime, anywhere. The DHA has taken bold steps to redefine
how we work collaboratively with the Department of Veterans Affairs (VA) and our civilian partners to improve
coordinated care for wounded warriors and all whom we have the honor to serve. More will be discussed on this
topic in Section V, Other Management Information, Initiatives, and Issues.
The DHA has developed four strategic goals:
Empower and Care for Our People
Optimize Operations across the Military Health System
Co-create Optional Outcomes for Health, Well-being and Readiness
Deliver solutions to Combatant Commands
The DHA leads the MHS integrated system of readiness and health to deliver the Quadruple Aim:
Increased Readiness – ensuring that the total military force is medically ready to deploy and that
the medical force is ready to deliver supportive health services anytime and anywhere in support
of the full range of military operations, including on the battlefield or disaster response and
humanitarian aid missions.
Better Care – continuing to advance health care that is safe, timely, effective, efficient, equitable,

Management’s Discussion and Analysis
4
and patient- and family-centered.
Better Health – improving the health of a population, making the transformation from health care
to health by reducing the generators of disease and injury, encouraging healthy behaviors,
increasing health resilience, and decreasing the likelihood of illness through focused prevention.
Lower Costs – increasing value by focusing on quality, eliminating waste, and reducing
unwarranted variation. In the move toward value-based health care, we begin to consider the total
cost of care over time, not just the cost of care at a single point in time. There are both near-term
opportunities to become more agile in our decision making and longer-term opportunities to
change the trajectory of cost growth by building value and improving the health of all we serve.
In fulfillment of Section 701 of the 2017 National Defense Authorization Act (NDAA), the DoD implemented the
most sweeping changes to the TRICARE benefit structure since TRICARE was established in 1995. Contract
management adjusted to synchronize these changes with the DoD’s transition to the TRICARE 2017 contracts and
regional oversight. The TRICARE changes expand beneficiary choice, improve access to network providers,
modernize beneficiary cost-sharing, and enhance administrative efficiency.
The TRICARE program provides healthcare services to 9.4 million beneficiaries. The most current generation of the
TRICARE Managed Care Support Contracts went into effect January 1, 2018, which established two TRICARE
regions in the United States, East and West, with a single contract for each region. Before January 1, 2018, the
private sector care contracts were organized into three geographical regions –North, South, and West. The current
generation merged the North and the South regions, now called the East region.
Contractors are responsible for managing the delivery of health care to TRICARE's beneficiaries by developing and
maintaining a civilian provider network consisting of both primary care and specialist providers. The contractors are
also responsible for ensuring adequate access to health care, referring and authorizing beneficiaries for health care,
educating providers and beneficiaries about TRICARE benefits, credentialing providers, and processing claims.
The DHA is the administrative agency for TRICARE. The Agency provides oversight, payment to and management
of claims processors, monitoring/management of the Improper Payments Information Act, and preparation of
consolidated financial statements and footnotes. It is responsible for the management of the dental program,
Uniformed Services Family Health Plans and pharmacy programs, both retail and mail order, and MERHCF.
Contract Resource Management
The CRM in Aurora, Colorado, under the leadership of J8, Deputy Assistant Director, Financial Operations, Mr.
Jeffrey Zottola, Chief Financial Officer, is responsible for the accounting, financial support, and financial reporting
for TRICARE's centrally funded private sector health care programs and the TRICARE Retail Pharmacy Refunds
Program. The CRM provides budget formulation input, carries out budget execution and prepares component
financial statements and footnotes.
In addition, CRM is responsible for processing invoices received electronically from its contractors, and through the
TRICARE Encounter Data Set (TEDS), and reporting these transactions through accessible electronic media. The
CRM provides funding availability certification and financial program tracking for the centrally funded private
sector care programs. The CRM monitors budget execution through analysis of current year and prior years spending
and program developments. It also assists the Contract Management division, Program Integrity (fraud), and Case
Recoupment activities related to private sector care.
CRM uses Defense Health Program (DHP) funds provided by annual appropriations from the Congress of the United
States to reimburse private sector health care providers for services rendered to TRICARE beneficiaries and funding
from MERHCF for the health care provided through TRICARE for Life (TFL) programs.
During the last two years of CRM’s operation, funding was received from the following sources:
Management’s Discussion and Analysis
5
CRM Funding Sources
Fiscal Year (FY) MERHCF Funding (Billions) Annual Appropriations (Billions) *
2018 $8.2 $14.4
2017 $8.4 $15.0
* CRM received Funding Authorization Documents (FADs) for FY17/1889 of $15.0 billion through September 30, 2017. CRM
received FADs for FY18/1889 of $14.4 billion through September 30, 2018.
Defense Health Program
The TRICARE program consists of a combination of MTFs and regional networks of civilian providers that work
together to provide care to 9.4 million eligible beneficiaries. The MTFs include 51 inpatient facilities and 628
medical and dental clinics, staffed by 144,217 MHS personnel, in the United States and overseas that, in conjunction
with the Uniformed Services University of the Health Sciences (USUHS), serve as premier training grounds for
military medical personnel. If care is not available in MTFs, beneficiaries seek care from civilian providers paid
through the TRICARE program via the Managed Care Support Contracts and the TFL program.
For FY 2017, the Consolidated Appropriations Act, 2017, Public Law No. 115-31, became law May 5, 2017,
providing DoD funding for FY 2017, replacing the Continuing Resolution in effect since the beginning of the fiscal
year.
For FY 2018, the Consolidated Appropriations Act, 2018, Public Law No. 115-141, became law March 23, 2018,
providing DoD funding for FY 2018, replacing the Continuing Resolution in effect since the beginning of the fiscal
year.
Covered beneficiaries include but are not limited to:
Active Duty Service Members and Families
National Guard/Reserve Members and Families
Retired Service Members and Families
Retired Reserve Members and Families
Survivors
Former Spouses
Medal of Honor Recipients and Families
Private Sector Health Care Plans
Individuals have access to different levels and types of benefits depending on their beneficiary status. Active Duty
Service Members (ADSM) generally obtain care from MTFs. When necessary, active duty personnel may obtain
care from civilian providers at government expense. Active Duty Family Members (ADFM) as well as military
retirees and dependents who are not eligible for Medicare can choose from one of two main options:
TRICARE Prime, a managed care option, is comparable to health maintenance organization
(HMO) benefits offered in many areas. Each enrollee chooses or is assigned a primary care
manager (PCM), a health care professional who is responsible for helping the patient manage his
or her care, promoting preventive health services (e.g., routine exams and immunizations), and
arranging for specialty provider services as indicated. TRICARE Prime access standards apply to
the travel time to reach a primary care or specialty care provider, waiting times to get an
appointment, and waiting times in doctors’ offices. TRICARE Prime’s point-of-service (POS)
option permits enrollees to obtain care from TRICARE-authorized providers other than the
assigned PCM without a referral, but with deductibles and cost shares significantly higher than
those under TRICARE Select (Formerly TRICARE Standard and TRICARE Extra). All
beneficiaries who are not ADSM or ADFM pay annual enrollment fees and network copayments.
TRICARE Prime offers fewer out-of-pocket costs than TRICARE Select, but less freedom of

Management’s Discussion and Analysis
6
choice in selecting providers.
TRICARE Select, .a self-managed, preferred-provider option for eligible beneficiaries (except
ADSMs and TFL beneficiaries) not enrolled in TRICARE Prime. Beneficiaries pay lower out-of-
pocket costs if care is provided by a TRICARE-authorized network provider. A fixed fee is paid
for care for most services from a TRICARE network provider instead of paying a percentage of
the allowable charge. Certain services can also be received from non-network, TRICARE-
authorized providers, but will result in paying higher cost sharing amounts for out-of-network
care. Effective January 1, 2018, TRICARE Select replaced TRICARE Standard and TRICARE
Extra.
In addition, the following plans are among those available:
TRICARE Prime Remote (TPR) is a managed care option for active duty service members and
their families who live and work in remote locations.
TRICARE Prime Overseas (Remote/Non-Remote) is a TRICARE Prime option offered in
remote and non-remote overseas locations for permanently-assigned active duty service
members or Guard/Reserve members and their dependents to receive care from a network of
licensed, qualified physicians. Beneficiaries enrolled in Prime Overseas will be assigned an MTF
PCM. There are no out-of-pocket costs as long as care is received from the PCM or with a
referral. Care received without a referral is subject to POS fees.
TRICARE Select Overseas provides comprehensive coverage in all overseas areas. This plan
allows beneficiaries to seek care from any civilian provider although prior authorization may be
needed from the overseas contractor. Costs vary based on the sponsor’s military status.
Beneficiaries will be reimbursed for a portion of the costs after paying co-payments and meeting
deductibles. Effective January 1, 2018, TRICARE Select Overseas replaced TRICARE Standard
Overseas.
TRICARE For Life (TFL) was created as wraparound coverage to Medicare-eligible military
retirees by Section 712 of the Floyd D. Spence National Defense Authorization Act for FY 2001
(P.L. 106-398). TFL functions as a secondary payer to Medicare, paying out-of-pocket costs for
medical services covered under Medicare for beneficiaries who are entitled to Medicare Part A
based on age, disability, or end-stage renal disease (ESRD). TFL serves as the final payer for
Medicare Covered Benefits, and first payer for TRICARE benefits that are not covered in the
Medicare, or other health care insurance programs.
TRICARE Reserve Select is a premium-based health plan that qualified Selected Reserve
members may select with benefits similar to TRICARE Select.
TRICARE Retired Reserves is a premium-based health plan that qualified Retired Reserve
members may select with benefits similar to TRICARE Select.
TRICARE Young Adult Program (TYA) is a premium-based health plan that implements the
NDAA of FY 2011, allowing coverage for adult children until age 26 in response to the Patient
Protection and Affordable Care Act of 2010 requiring civilian health plans to offer such coverage.
TRICARE Pharmacy Program is a program that provides low cost pharmaceutical drugs to
TRICARE beneficiaries in MTFs, via TRICARE retail network pharmacies and through the
TRICARE Pharmacy Home Delivery Program (for CRM, this program may also be called
TRICARE Mail Order Pharmacy (TMOP)).
TRICARE Active Duty Dental Program (ADDP) is a program offered to TRICARE Active Duty
beneficiaries at military dental treatment facilities or civilian dental services. There are also two
premium-based programs: TRICARE Dental Program (TDP), which includes ADFMs, and
TRICARE Retiree Dental Program (TRDP).
Health Care Purchased From Civilian Providers
Claims for care provided by civilian providers are submitted to claims processors who work for the private sector,
managed care contractors. Claims are adjudicated to ensure that the patients are eligible, that care was provided by
authorized healthcare providers, for covered benefits and for the right price. A record of the transaction is submitted
to DHA in the form of a TEDS file. The TEDS records are run through a series of automated edits to ensure that the

Management’s Discussion and Analysis
7
data is accurate and that data standards are met. If the TEDS records pass these edits, the records are accepted, and
payment to the contractor is authorized.
In addition to payments made to contractors through the TEDS record process, TRICARE contractors are paid based
upon invoices that are submitted to CRM. The invoices are for administrative services provided for the management
of the healthcare benefit, such as the operation of TRICARE Service Centers, network development operations,
provider education services and other services that are non-healthcare in nature.
In addition to the direct healthcare/MTF systems and the private sector healthcare systems, DoD beneficiaries may
enroll in capitation rate plans in specific locations where Uniformed Services Family Health Plan (USFHP) facilities
are available. These plans include inpatient and outpatient services and a pharmacy benefit. The capitation rate is
paid by DoD. Beneficiaries who choose enrollment in these plans are ineligible for care in MTFs as well as benefits
under the TFL programs.
Medicare Eligible Retiree Health Care Plans
The FY 2001 NDAA significantly expanded the DoD health care benefits for Medicare-eligible military retirees,
their dependents and survivors. The NDAA established the TRICARE Pharmacy Program that began on April 1,
2001, and the TFL benefits that became effective on October 1, 2001.
The TRICARE Pharmacy Program authorizes eligible beneficiaries to obtain low-cost prescription medications from
TMOP and TRICARE network and non-network civilian pharmacies. Beneficiaries may also continue to use
military hospital and clinic pharmacies, at no charge.
Beneficiaries who are eligible for the Medicare program (over 65, End-Stage Renal Disease, survivors, etc.) can
receive care from Medicare participating providers through the TFL program. With this program TRICARE serves
as the final payer to Medicare and other health insurance for Medicare covered benefits, and first payer for
TRICARE benefits that are not covered by Medicare or other health insurance programs.
In accordance with DoD 7000.14-R, Financial Management Regulation, Volume 12, Chapter 16, CRM reports daily
obligations to MERHCF for healthcare purchased from civilian providers or “purchased care”. Daily claims are
validated by the voucher edit procedures required by the TRICARE/Civilian Health and Medical Program of the
Uniformed Services (CHAMPUS) Automated Data Processing Manual 6010.50-M, dated May 1999, to ensure that
only costs attributable to Medicare-eligible beneficiaries are included in payments drawn from MERHCF.
II Performance Measures
The Evaluation of the TRICARE Program: Fiscal Year 2018 Report to Congress Access, Cost, and Quality Data
through Fiscal Year 2017, reflects DHA’s mission and vision statements, updates and refines descriptions of core
values, and presents key results of the metrics supporting DHA’s Strategic Plan that focuses on how DHA defines and
measures mission success, and how DHA plans to continuously improve performance.
Stakeholder Perspective*
The $53.64 billion Unified Medical Program (UMP) presented in the FY 2018 President’s Budget,
including estimated outlays from MERHCF, is 3% higher that the FY 2017 actual expenditures, and
is 9% of total estimated DoD outlays.
The number of beneficiaries eligible for Department of Defense (DoD) medical care remained at
approximately 9.4 million between FY 2015 and FY 2017. The number of Prime-enrolled
beneficiaries has decreased annually since 2011, falling to 4.8 million in FY 2017, consistent with
the decrease in Active Duty and their family members.
TYA enrollment increased to just under 40,000 beneficiaries under age 26 enrolled in FY 2017, from
just over 38,000 in FY 2016. Prime enrollment was 43% of the total.
TRICARE Reserve Select (TRS) enrollment increased in FY 2017 to over 145,000 plans and almost
386,000 covered lives, while retired Reservists and their families in TRICARE Retired Reserve
(TRR) reached just over 3,000 plans and 8,100 covered lives.

Management’s Discussion and Analysis
8
MHS Workload and Cost Trends*
The percentage of beneficiaries using MHS services remained about the same between FY 2015 and
FY 2017, at between 85-86%.
Excluding TFL, total MHS workload (direct and purchased care combined) fell from FY 2015 to FY
2017 for inpatient care (-3%) and prescription drugs (-2%). Total outpatient workload increased by
1%.
From FY 2015 to FY 2017, direct care workload decreased for inpatient care (-6%) and prescription
drugs (-1%), but increased by 2% for outpatient care. Over the same period, direct care costs rose by
5%.
Excluding TFL, purchased care workload fell for inpatient care (-2%), outpatient care (less than 1%),
and prescription drugs (-4%). Overall, purchased care costs decreased by 8%, due largely to the
resolution of fraudulent compound drug prices at the end of FY 2015.
The purchased care portion of total MHS health care expenditures decreased from 55% in FY 2015
to 52% in FY 2017.
In FY 2017, out-of-pocket costs for MHS beneficiary families under age 65 were between $5,700
and $7,200 lower than those for their civilian counterparts, while out-of-pocket costs for MHS senior
families were $3,100 lower.
Lower Cost*
MHS estimated savings include nearly $850 million in retail pharmacy refunds in FY 2017 and $105
million in Program Integrity (PI) activities in calendar year 2016.
Increased Readiness*
Force Health Protection: At the end of FY 2017, the overall medical readiness of the total force
was at 87%, with the Active Component at 88% and the Reserve Component at 85%, all equaling or
exceeding the strategic goal of 85%. Dental readiness, at 96%, exceeded the MHS goal of 95%. The
MHS surgical community is leading the way in identifying and enumerating critical clinical
readiness skill sets.
Better Care*
Access to Care: In FY 2017, about 84% of Prime enrollees reported at least one outpatient visit,
comparable to the civilian HMO benchmark, while administrative data reflect 82% of non-Active
Duty enrollees had at least one recorded primary care visit and 40% had five or more visits. Patient-
Centered Medical Home (PCMH) primary care administrative measures indicate MTF enrollees saw
their primary care provider 59% of the time, and a PCMH team member 92% of the time; days to
their next 24-hour or acute appointments declined to 0.93 days [less than one day], and continued to
meet the seven-day standard for future appointments. Beneficiary enrollment in and usage of secure
messaging continued to increase in FY 2017. Dispositions and bed-days per 1,000 enrollees
continued to improve, decreasing 26% and 27%, respectively, from FY 2012. The new standardized
DHA/Service survey of beneficiary outpatient experience shows strong and stable ratings of access
to care at 83%.
Hospital Quality of Care: MTFs and MHS-supporting civilian hospitals report results are
comparable to many Joint Commission national hospital quality measures and consistent with the
national Joint Commission benchmarks in the perinatal care measures.
Outpatient Care: MHS Healthcare Effectiveness Data and Information Set (HEDIS
®
) rates exceed
the national standards at the 90
th
percentile for colorectal cancer screening, mental health follow-up
visits post hospitalization, and treatment of children with upper respiratory infection, and surpass the
national 75
th
percentile for cervical cancer screenings, low back pain, well-child visits, and treating
children for pharyngitis.
Beneficiary Ratings of Inpatient Care:
o Overall Hospital Rating: Direct care has shown improved patient hospital ratings from FY
2015–2017, with Service meeting or exceeding the national Hospital Consumer Assessment
of Healthcare Providers and Systems (HCAHPS) benchmark in the medical and surgical
product lines. While ratings continue to improve in the obstetric product line for all
Services and purchased care, they remain below the HCAHPS benchmark.
Management’s Discussion and Analysis
9
o Beneficiary Recommendation of Hospital: MHS beneficiary ratings for both direct and
purchased care are above the HCAHPS benchmark in the medical and surgical product line,
while Service and purchased care ratings are close to or above the national HCAHPS
benchmark in FY 2017 for the obstetric product line.
Patient Safety: The MHS direct care system has been focusing on reducing Wrong-Site Surgery
Sentinel Events (WSS SEs) through the development and dissemination of prevention tool kits,
educational webinars, leadership engagement and direct MTF coaching. Compared to FY 2016, FY
2017 saw a 32% reduction in WSS SEs.
MHS Provider Trends: The number of TRICARE network providers increased by 21% from FY
2013 to FY 2017. The total number of participating providers increased by 9% over the same time
period.
Access for TRICARE Standard/Extra Users: Results from the first year of the congressionally
mandated four-year survey (2017–2020) of civilian providers and MHS non-enrolled beneficiaries
shows 8 of 10 physicians accept new TRICARE Standard patients, a higher acceptance rate than
reported for behavioral health providers.
*Note: Source of all metrics presented above is the Evaluation of the TRICARE Program: Fiscal Year
2018 Report to Congress Access, Cost, and Quality Data through Fiscal Year 2017.
III Analysis of Financial Statements
Comparative Financial Data
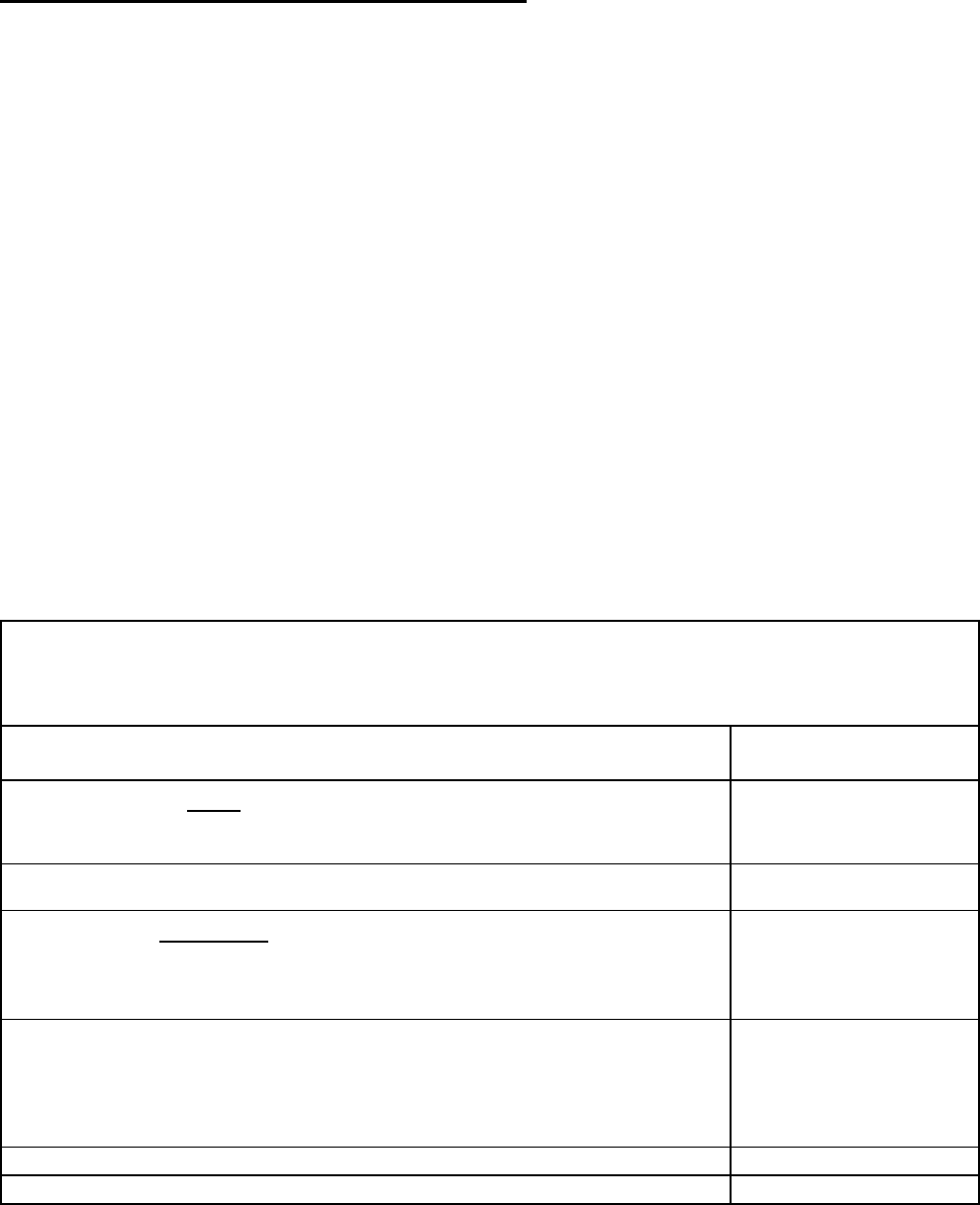
The following table presents comparative financial statement information for CRM.
Contract Resource Management
Table of Key Measures
for the years ended September 30, 2018 and 2017
($ in Thousands) Current FY Prior FY Increase/ (Decrease)
$ %
Costs
1
Total Financing Sources
$14,729,933 $14,589,443
$140,490 1.0%
Less: Net Cost
$9,274,571 $22,931,861
($13,657,290) -59.6%
Net Change of Cumulative Results of
Operation $5,455,362 (8,342,418) $13,797,780 165.4%
Net Position
2
Assets:
Fund Balance with Treasury $1,393,187 $1,675,116 ($281,929) -16.8%
Accounts Receivable $448,729 $340,194 $108,535 31.9%
Total Assets $1,844,152 $2,015,329 ($171,177) -8.5%
Liabilities:
Accounts Payable ($492,098) ($340,280) $151,818 44.6%
Military Retirement & Other Federal
Employment Benefits ($179,548,375) ($184,901,446) ($5,353,071) -2.9%
Total Liabilities ($180,042,709) ($185,241,745) ($5,199,036) -2.8%
Net Position (178,198,557) (183,226,416) $5,027,859 2.7%
1
Source: Statement of Net Cost and Statement of Changes in Net Position
2
Source: Balance Sheet

Management’s Discussion and Analysis
10
Total Financing Sources
Total Financing Sources increased by $140.5 million (1%) because of an increase in residual payments for FY17
disbursed in FY18, along with cost increases for Phase In/Out costs and incentives under the Managed Care Support
contracts.
Net Cost
Total Net Cost of Operations decreased $13.7 billion (60%) for the reasons noted below.
Total Costs
Intragovernmental costs decreased $87.2 million (11%) due to decreases in the TMOP benefit program of $87.0 million
and Air Force collection costs of $1.5 million, offset by an increase in Department of Justice (DoJ) - Case Recoupments
of $0.4 million accounting for 101% of the decrease.
Public costs, other than losses/gains from actuarial assumption changes, decreased $2.5 billion (18%) due to a net
decrease in expenses before losses/(gains) from actuarial assumption changes of $2.7 billion, 108% of the decrease.
Losses/(gains) from actuarial assumption changes decreased $10.8 billion (120%) (see below).
The actuarial liability for Military Pre Medicare-Eligible Retiree Health Benefits has three components that affect net
cost. The first, Costs Other than Losses/Gains from Actuarial Assumption Changes, mentioned above, decreased $2.5
billion. The second, Losses/(Gains) from Actuarial Assumption Changes decreased $10.8 billion and the third, Benefit
Outlays, increased $0.2 billion, netting to a decrease in actuarial expenses of $13.5 billion. The actuarial liability is
discussed in detail in Note 9.
Total Revenue
Total earned revenue increased $256.5 million (26%). Intragovernmental revenue increased $7.1 million (1%)
attributable to an increase in revenue from the Coast Guard of $5.1 million, PHS of $1.5 million, and NOAA of $0.4,
accounting for 99% of the increase.
Public revenue increased $249.4 million (58%) attributable to an increase in revenue from TRS of $8.3 million and
Prime Enrollment Fees of $241.3 million, accounting for 100% of the increase.
Net Change in Cumulative Results of Operation
Net Change in Cumulative Results of Operation increased $13.8 billion (165%) due to an increase in financing sources
and a decrease in net costs as discussed above.
Funds Balance with Treasury (FBWT)
FBWT decreased $281.9 million (17%). The decrease is attributable to obligations not yet disbursed of $395.8 million
and programmatic FAD decreases of $626.4 million, offset by a decrease in obligations of $550.7 million, net
appropriation exchanges of $37.1 million, and FAD returns and deobligations of $141.6 million, accounting for 104%
of the decrease.
Accounts Receivable
Accounts Receivable increased $108.5 million (32%).
Federal Accounts Receivable increased $6.2 million (14%) attributable to increases in billings to the Coast Guard of
$5.6 million and to the PHS of $0.7 million, accounting for 100% of the increase.

Management’s Discussion and Analysis
11
Non-Federal Accounts Receivable increased $102.3 million (35%), attributable to an increase in Other Receivables of
$116.8 million offset by a decrease of $14.5 million in the TRICARE Retail Pharmacy Refunds Program.
The decrease in the TRICARE Retail Pharmacy Refunds Program is due to decreases in routine billings and pharmacy
collections. The accounts receivable balance at year end is also affected by the timing of billings and collections as well
as the calculated accrual.
The increase in Other Receivables of $116.8 million, mentioned above, was primarily due to net increases in Office of
General Counsel (OGC) cases of $62.3 million, contractor held debt of $19.5 million, and TEDS claims/TRICARE
Claims Management (TCM) and other of $37.4 million, accounting for 102% of the increase.
Total Assets
Total Assets decreased $171.2 million (9%), primarily due to the decrease in Funds Balance with Treasury of $281.9
million offset by an increase in Accounts Receivable of $108.5 million.
Accounts Payable
Accounts payable increased $151.8 million (45%), primarily attributable to increases in the Managed Care Support
contract of $72.2 million, MTF Enrollees of $12.8 million, Supplemental Health Care of $12.2 million, Active Duty
Dental of $9.4 million, and Capital and Direct Medical Education Costs of $38.4 million, totaling $145.0 million, 96%
of the increase.
Military Retirement and Other Federal Employment Benefits
Annually, the DoD Office of the Actuary (OACT) calculates this actuarial liability at the end of each fiscal year using
the current active and retired population plus assumptions about future demographic and economic conditions.
Note 9 of the financial statements reflects two distinct types of liabilities related to Military Retirement and Other
Federal Employment Benefits. The line entitled “Military Pre Medicare–Eligible Retiree Health Benefits” represents
the actuarial (or accrued) liability for future health care benefits that are not yet incurred. The line entitled “Other”
represents the incurred-but-not-reported reserve amount which is an estimate of benefits already incurred but not yet
reported to DoD for all DHP beneficiaries excluding those from the retiree population.
The DHA actuarial liability is adjusted at the end of each fiscal year. The 4
th
Quarter, FY 2018 balance represents the
September 30, 2018 amount.
Total Liabilities
Total Liabilities decreased $5.2 billion (3%), primarily due to the decrease in Military Retirement and Other Federal
Employment Benefits, the actuarial (or accrued) liability for future health care benefits that are not yet incurred
discussed above.
Net Position
Net Position decreased $5.0 billion (3%), due to the net decreases discussed above.
IV Analysis of Systems, Controls and Legal Compliance
Systems
CRM is positioned to achieve positive audit results due to exceptions granted to the program by the U.S. Treasury; the
U.S. Treasury prepares disbursements from data directly submitted by CRM. The Purchased Care Program managed by
CRM includes an immense volume of claims processed by two regional Health Care contractors, the TRICARE Dual
Eligible Fiscal Intermediary (TDEFIC) contractor, a foreign claims contractor, and a pharmaceutical contractor to

Management’s Discussion and Analysis
12
process retail and mail order prescriptions. Contract amendments are made to incorporate policy or administrative
changes, as needed.
To track these programs, CRM uses the TEDS, a financial feeder system, through which all claims are processed to
Oracle Federal Financials (OFF). OFF contains TCM, Accounts Receivable, Accounts Payable, Purchase Orders and
the General Ledger modules. CRM sends OFF trial balances to the Defense Finance and Account Services-Indianapolis
(DFAS-IN), through the Defense Department Reporting System-Budgetary (DDRS-B), who reviews the balances for
proprietary to budgetary adjustments, prepares journal vouchers in DDRS and compiles the financial statements.
The initiative to improve controls, increase efficiency, and documentation are contributing factors in the reduction of
the risks and misstatements that can occur within FBWT. The risk areas are monitored ensuring prompt action if
fluctuation occurs. Many processes are automated, so it is important to consider information systems and the effects on
inherent risk. The asserted inherent risk revealed from the test samples indicated the risk components are susceptible to
a material misstatement in the area of:
Improper payments
Inaccurate claims paid
Unauthorized reimbursed claims
Inaccurate electronic postings
Incorrect number or amount of claims transmitted
Discrepancies between the U.S. Treasury and CRM
Intragovernmental Payment and Collection (IPAC) amounts not accurately reported to the U.S.
Treasury
The CRM has established consistent business rules for management control impacting disbursing and collection
activities, and the related banking and U.S. Treasury reconciliations.
With processes and procedures in place and the continued risk monitoring, monthly reconciliations are performed to
ensure balances reconcile to the U.S. Treasury on a monthly, quarterly, and fiscal year basis.
The CRM uses OFF to track commitments and obligations for its purchases. These transactions flow through the CRM
Unadjusted Trial Balance that is submitted to DFAS-IN and becomes the primary source into the financial statements.
The DoD recognizes the significance and impact of Financial Management Systems (FMS) in obtaining unmodified
audit opinions, as evidenced by implementation of the Standard Financial Information Structure (SFIS) and Assertion
Package Tabs that focus on FMS and key feeder systems. CRM continues to improve financial management and feeder
system processing and eliminate weaknesses.
The CRM is responsible for implementing and maintaining FMS that substantially comply with Federal financial
management system requirements, Federal accounting standards, and the United States Standard General Ledger
(USSGL) at the transaction level. The CRM determined that the FMS substantially complied with the Federal financial
management systems requirements, Federal accounting standards, and application of the USSGL at the transaction level
as of September 30, 2018.
The September 2007 Defense Business Systems Management Committee (DBSMC) resulted in the Investment Review
Board (IRB) directing the DHA E-Commerce System (DHA ECS) program, as a Target Accounting System, to
“comply with the OUSD (C) memorandum, ‘SFIS Implementation Policy’ dated August 4, 2005.” The DHA achieved
SFIS compliance during FY 2011. The DHA continued to maintain SFIS compliance through FY 2018. In addition, the
IT management and technical staff prepared for an SFIS compliance assessment conducted by the DoD Joint
Interoperability Test Center during FY 2017 and FY 2018. Corrective actions for all findings were implemented by
October 1, 2018.

Management’s Discussion and Analysis
13
TEDS
TEDS is the entry point from the Health Care Support Contactors. The data includes various categories of records that
include Institutional, Non Institutional, and Provider health plan information. TEDS is primarily required by DHA to
account for the expenditure of government funds and to develop statistical information used for analysis by DHA for
reporting to the Congress of the United States, the Executive Branch, for developing trends and budget projections and
for determining the loss to the government when DoJ institutes criminal or civil action against a provider who has been
under investigation. During FY 2018, the TED Production environment was hosted at two different locations:
October 1, 2017 - June 22, 2018 Defense Information System Agency Oklahoma City (DISA-OKC)
June 23, 2018 - Present - Defense Information System Agency San Antonio (DISA-SATX).
Statement on Standards for Attestation Engagements (SSAE) No. 18, Service Organization Control (SOC) reports are
available for the TRICARE Manage Care regional contracts – West (Health Net Federal Services) and East (Humana
Military Healthcare), along with their subcontractors’ claims processing organizations, West (Palmetto Government
Benefit Administrators (PGBA)) and East (Wisconsin Physicians Services (WPS)). SOC reports are also available for
the Mail Order and Retail Pharmacy (TPharm-Express Scripts), TDEFIC (WPS), Pharmacy Data Transaction Services
(PDTS) (Change Healthcare), and the TRICARE Overseas Program (International SOS Government Services, Inc.
(ISOS)) as well as its subservice organization (WPS).
Once claims enter the claims processing systems at the various contractors, they are subjected to various edits including
patient eligibility (verified via the Defense Enrollment Eligibility Reporting System (DEERS)), regional or TDEFIC
eligibility, and provider eligibility. If the claims pass those edits, the benefit calculations occur based on programmed
payment rules and reimbursement methods determined by TRICARE. The claims processing systems are able to
determine the appropriate reimbursement methodology based on information included in the claims such as type of
service, provider record, claim form type, etc.
On a daily basis, the contractors submit the claims that successfully pass their edits as TEDS records to DHA. The
incoming TEDS are required to pass another set of edits in-house at DHA before they are accepted and paid.
As reported during previous fiscal years, the TED application, which is a major claims-based feeder system for the
CRM financial statements, did not have a continuity of operations recovery site (COOP). DHA however, had been
working on a substantial project to migrate this application to DISA managed platforms to resolve these technical and
COOP related issues. Phase 1 of this effort was completed on August 22, 2017 when the TED system was migrated
from ageing outdated technology to a newer internal cloud-based hosting service platform at DISA-OKC.
The second phase of the migration was initiated on June 22, 2018, wherein the Production environment for TED was
copied from DISA-OKC to DISA-SATX. Upon completion of this effort, the environment hosted at DISA-OKC
became the COOP Platform supporting any Disaster Recovery requirements. Since this phase is complete TED has an
operational COOP site and DHA-CRM closed this associated risk.
E-Commerce
The DHA ECS is an integrated, centralized major system that improves DHA’s core financial, contracting and business
processes by providing a seamless integrated financial and contracting system. It uses commercial off-the-shelf
(COTS) software and hardware to provide a network-based, multi-user system with the essential tools to manage and
administer the TRICARE financial and contracting activities. The core financial solution embedded in the DHA ECS,
OFF, is a Financial Systems Integration Office (FSIO) (formerly known as the Joint Financial Management
Improvement Program [JFMIP]) certified financial system. This component is integrated with a contract management
component and a management control component. The management control component enables Web-based queries of
TRICARE contracting and financing information directly against a single database and permits direct reporting of
program status and tracking information to management.

Management’s Discussion and Analysis
14
OFF
OFF is the financial subsystem of the DHA ECS. It supports budget and accounting/finance functions and healthcare
(TEDS) claims processing. Since 2009, the OFF financial subsystem has employed DISA hardware at the OKC data
center.
The accounting/finance function provides support for activities associated with establishing and administering the
accounting classification structure, the standard general ledger and subsidiary account structure. The accounting
function interfaces with the contracting functions to obtain contract data for issuing payments and maintaining financial
records. OFF is used by CRM and OGC for debt management. It uses external and internal interfaces to provide
financial reports, make payments and to provide management information to other federal government agencies,
financial agencies and institutions.
The healthcare (TEDS) claims processing function is performed by the OFF-TCM extension. TCM is a custom built
extension to OFF which converts healthcare (TEDS) data into financial data that can then be processed by standard
(COTS) OFF. The TCM conversion of healthcare data is of critical importance to the accuracy of the financial
information presented in the CRM financial statements. TRICARE processed about 186 million claims (invoices)
valued at approximately $18.4 billion during FY 2018. The financial conversion, processing and posting of TEDS data
from commitment/obligation through payable/receivable is 100% automated. In addition to creating budgetary and
accounting transactions, TCM supports the TEDS system by providing daily financial data to TEDS. Without the data
received from the OFF-TCM extension the TEDS system would be unable to process and properly edit the contractor’s
daily data submissions. TEDS functions supported by the OFF-TCM data provided include:
header and detail data editing used for government acceptance of services
funds control at both the commitment and obligation level
prevention of duplicate billings at the header level
The Organizational Execution Plan (OEP) and investment certification process resulted in the Weapon System Life
Cycle Management/Materiel Supply and Services Management (WSLM/MSSM) Investment Review Board (IRB)
recommending a conditional approval. The IRB required DHA to submit an assessment as to whether the system
performs acceptance activities for unclassified Federal Acquisition Regulation (FAR) based contract/orders, and
provides a plan for receiving associated invoice/shipment data from the Invoicing, Receipt, Acceptance and Property
Transfer (iRAPT) system (formerly known as Wide Area Workflow [WAWF]) and posting acceptance data.
During Q3 FY 2017, the DHA ECS program technical staff deployed all OFF application software interface and
configuration changes associated with the iRAPT interface project. Activation of the Global Exchange (GEX) support
of the interface is fully functional.
The OFF application is a current; fully supported Version of R-12. The DHA ECS program successfully deployed the
Version R-12 technical upgrade in January 2016. The CRM remains compliant through FY 2018.
As main participants of the TRICARE Retail Pharmacy Refund Program, MERHCF/DHA-CRM, along with the Health
Care Data Analysis (HCDA) Group, receive and use pharmacy files as a basis for demand letters, billing and invoicing,
the calculation of penalties, interest and administrative costs, and dispute tracking. Using existing E-Commerce
toolsets, the Pharmacy Modernization Project was deployed in FY 2015 to streamline billings, collections,
reconciliations, dispute resolutions, and pricing changes. Since deployment of the Pharmacy Modernization Project
collections have increased significantly to an average of 98% p
er bill quarter.
During FY 2018, the DHA ECS Program continued to sustain and enhance all deployed phases through Phase IV of the
Pharmacy Modernization Project. Development efforts for Phase V, which is expected to further streamline the dispute
resolution process, is planned for FY 2019.
Controls & Legal Compliance
The CRM is responsible for understanding and complying with applicable provisions of laws, regulations, and
contracts, including those that affect the financial statements. The CRM is not aware of any undisclosed pending or

Management’s Discussion and Analysis
15
threatened litigation, claims, and assessments, the effects of which should be considered when preparing the financial
statements. There are no known:
Violations or possible violations of laws or regulations, the effects of which should be disclosed in the
financial statements or as a basis for recording a loss contingency.
Material liabilities or gain or loss contingencies that are required to be accrued or disclosed that have
not been accrued or disclosed.
Unasserted claims or assessments that are probable of assertion and must be disclosed that have not
been disclosed.
Anti-Deficiency Act, 31 U.S.C. §§ 1341, 1342, 1350, 1351, 1517: ANTI-DEFICIENCY ACT
The Anti-deficiency Act (ADA) prohibits federal employees from obligating in excess of an appropriation, before funds
are available or from accepting voluntary services. As required by the ADA, DHA-CRM notifies all appropriate
authorities of any ADA violations. The DHA-CRM management has taken and continues to take necessary steps to
prevent ADA violations. Investigations of any violations will be completed in a thorough and expedient manner. The
DHA-CRM remains fully committed to resolving ADA violations appropriately and in compliance with all aspects of
the law. The CRM is not aware of any violations of the Anti-deficiency Act that must be reported to the Comptroller
General, Congress, and the President for the year ended September 30, 2018.
Prompt Payment Act, 31 U.S.C. §§ 3901-3907; Prompt Payment Act
In 1982, Congress enacted the Prompt Payment Act (PPA) to require federal agencies to pay their bills on a timely
basis, to pay interest penalties when payments are made late, and to take discounts only when payments are made by the
discount date. DHA-CRM uses iRAPT (formerly WAWF) system to ensure compliance with this statutory requirement.
Provisions Governing Claims of the United States Government as provided in 31 U.S.C. §§ 3711-3720E (including
provisions of the Debt Collection Improvement Act of 1996, (DCIA), as amended by the Digital Accountability and
Transparency Act of 2014); Debt Collection Improvement Act of 1996
The Debt Collection Improvement Act of 1996 (DCIA), as amended by the DATA Act, requires that Federal agencies
refer delinquent debts to Treasury within 120 days and take all appropriate steps prior to discharging debts. DHA-CRM
follows applicable requirements for establishing and collecting validated debts, ensuring compliance with Debt
Collection statutes and regulations.
Digital Accountability and Transparency Act of 2014 (DATA Act), 31 U.S.C. § 6101 note. The DATA Act amended the
Federal Funding Accountability and Transparency Act of 2006 (FFATA). DIGITAL ACCOUNTABILITY AND
TRANSPARENCY ACT OF 2014
The Digital Accountability and Transparency Act of 2014 (DATA Act) expands the Federal Funding Accountability
and Transparency Act of 2006 to increase accountability and transparency in federal spending, making federal
expenditure information more accessible to the public. It directs the Federal Government to use government-wide data
standards for developing and publishing reports and to make more information, including award-related data, available
on the USASpending.gov Web site. The standards and Web site allow stakeholders to track federal spending more
effectively. Among other goals, the DATA Act aims to improve the quality of the information on USASpending.gov, as
verified through regular audits of the posted data, and to streamline and simplify reporting requirements through clear
data standards. DHP Enterprise complies with the DATA Act; making its expenditures accessible to the public on
USASpending.gov.
Management Assurances
The Federal Managers’ Financial Integrity Act (FMFIA) requires agencies to assess the effectiveness of internal control
and provide an annual statement of assurance regarding internal accounting and administrative controls, including
controls in program, operational, and administrative areas as well as accounting and financial reporting. The DHA-
CRM conducted its assessment of risk and internal control in accordance with the Office of Management and Budget
(OMB) Circular No. A-123, Management’s Responsibility for Enterprise Risk Management and Internal Control
and

Management’s Discussion and Analysis
16
the Green Book, Government Accountability Office (GAO)-14-704G, Standards for Internal Control in the Federal
Government. Based on the results of its assessment, DHA-CRM can provide reasonable assurance that internal controls
over operations, reporting, and compliance were operating effectively as of September 30, 2018.
The DHA-CRM conducted its assessment of the effectiveness of internal controls over operations in accordance with
OMB Circular No. A-123, the GAO Green Book, and the FMFIA. Based on the results of this assessment, the DHA-
CRM can provide reasonable assurance that internal controls over operations, reporting, and compliance were operating
effectively as of September 30, 2018.
The DHA-CRM conducted its assessment of the effectiveness of internal controls over reporting (including internal and
external financial reporting) in accordance with OMB Circular No. A-123, Appendix A. Based on the results of this
assessment, the DHA-CRM can provide reasonable assurance that the internal controls over operations, reporting
(including internal and external financial reporting as of September 30, 2018), and compliance were operating
effectively as of September 30, 2018.
The DHA-CRM also conducted an internal review of the effectiveness of the internal controls over the integrated
financial management systems in accordance with Federal Financial Management Improvement Act (FFMIA) of 1996
(Public Law 104-208) and OMB Circular No. A-123, Appendix D. Based on the results of this assessment, the DHA-
CRM can provide reasonable assurance that the internal controls over the financial systems are in compliance with the
FFMIA and OMB Circular No. A-123, Appendix D, as of September 30, 2018.
Status of Audit Findings
Consistent with government-wide financial reform and the President’s Management Agenda, one of the goals of DoD is
to improve operational, day-to-day accounting and financial management, and achieve an unmodified audit opinion on
each DoD component’s financial statements. This requires Military Departments, Defense Agencies, and other DoD
Components that are required to prepare financial statements, to develop and implement broad improvement plans and
take appropriate actions to achieve and maintain unmodified audit opinions.
The CRM received unmodified opinions for FY 2010 through FY 2018. FY 2017 and FY 2018 had no reportable
conditions and, as such, there are no status updates for reportable conditions.
DHA Program Integrity Office
The DHA Office of Program Integrity (PI) manages anti-fraud and abuse activities for the DHA to safeguard
beneficiaries and protect benefit dollars. The PI responsibilities include:
Central coordinating office for allegations of fraud and abuse within the TRICARE Program.
Develops and executes anti-fraud and abuse policies and procedures.
Provides oversight of contractor program integrity activities.
Develops cases for criminal prosecutions and civil litigations.
Coordinates investigative activities with Military Criminal Investigative Offices, as well as other
federal, state, and local agencies.
Initiates administrative measures
DHA PI had another active year in supporting ongoing investigative actions. During calendar year 2017, 690 active
investigations were managed, 304 new cases were opened, and 1,086 leads/requests for assistance were responded to.
DHA PI received and evaluated 451 new qui tams. A qui tam is a provision of the Federal Civil False Claims Act
(FCA) that allows private citizens, known as relators, to file lawsuits in the name of the U.S. Government alleging that
private companies—usually their employer—have submitted fraudulent claims for government payment. The private
whistleblowers who file these qui tam lawsuits receive a percentage of the settlement or judgment amount if a
settlement or judgment is reached. For more information, please refer to DHA’s “Program Integrity Operational
Report” dated January 1, 2017 through December 31, 2017. The FY 2018 data will not be available until published in
April 2019, due to the time required to compile 4th Quarter, FY 2018 data.

Management’s Discussion and Analysis
17
V Other Management Information, Initiatives, and Issues
TRICARE Standard Discount Program (SDP) formerly known as Mandatory Agreements Retail Refunds (MARR)
The SDP (Program 006) is a Standard or Minimum Refund, formerly known as MARR, on a Section 703 Covered
Drug. It is by law equal to the difference between Non-Federal Average Manufacturer Price (Non-FAMP) and Federal
Ceiling Price (FCP) (FCP = 76% x Non-FAMP).
The NDAA for FY 2008, §703 enacted 10 U.S.C. 1074g(f) which mandated all covered TRICARE Retail Pharmacy
Network prescriptions filled after January 28, 2008, be subject to FCP.
The initial rule, published in the Code of Federal Regulations at 32 C.F.R. 199.21(q), subjected the TRICARE retail
pharmacy program to pricing standards known as FCP by prohibiting pharmaceutical manufacturers from receiving
more than the FCPs for pharmaceuticals purchased by DoD for the TRICARE retail pharmacy program.
The OGC requested waiver/compromise authority from DoJ, received it, and has resolved all pending
waiver/compromise requests applicable to the “Retro Period” (January 2008 through June 2009) based upon the
provisions of 32 C.F.R. §199.11.
TRICARE Additional Discount Program (ADP) formerly known as Voluntary Agreements Retail Rebates (VARR)
The DHA initiated a new retail pharmacy rebate program during FY 2007, ADP, formerly known as VARR.
Manufacturers may offer rebates to the DoD for pharmaceutical agents dispensed through the TRICARE Retail
pharmacy network. The Uniform Formulary VARR (UF-VARR) is contingent upon pharmaceutical agents being
included on the 1
st
(generic drugs) or 2
nd
(formulary brand drugs) tiers of the DoD Uniform Formulary. There are two
types of additional discounts:
ADP #1 (Program 009) - WAC (% of Wholesale Acquisition Cost): The manufacturer’s list price for
the drug to wholesalers or direct purchasers in the United States, not including prompt pay or other
discounts, rebates or reductions in price, as reported in wholesale price guides or other publications
of drug pricing data.
ADP #2 (Program 010) – (FCP - additional discount): The maximum price the manufacturer can
charge for a Federal Supply Schedule (FSS) listed drug to the Big 4 - VA, DoD, PHS, and the Coast
Guard; calculated annually by VA using Non-FAMP and other data submitted by the manufacturer.
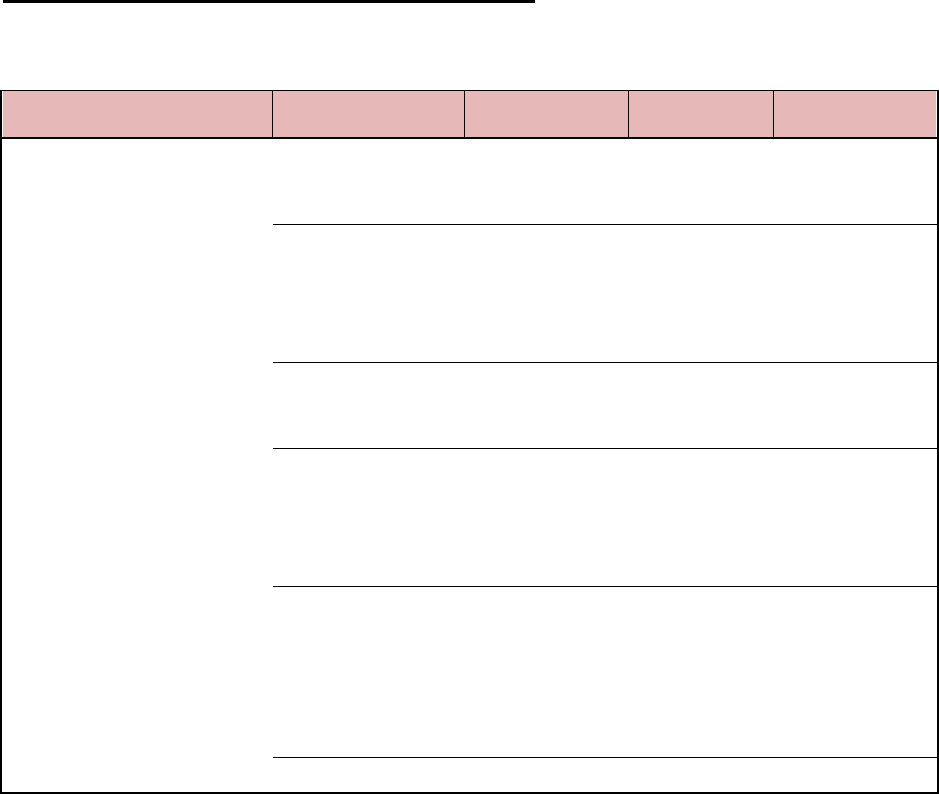
The table on the following page highlights DoD activity since the inception of the Program. DoD has collected $12.0
billion to date and continues rigorous collection efforts for both programs.
Management’s Discussion and Analysis
18
TRICARE Retail Pharmacy Refunds Program
Program To Date (CY 2008-
3rd Quarter, CY 2018 Total DHP Non-DoD MERHCF
SDP -
Billed $7,767,316,589 $3,533,064,654 $119,650,058 4,114,601,877
Collected (7,468,113,084) (3,403,791,255) (114,168,670) (3,950,153,159)
Net 299,203,505 129,273,399 5,481,388 164,448,718
ADP -
Billed 4,745,537,027 2,151,949,586 73,985,370 2,519,602,071
Collected (4,543,283,635) (2,063,943,291) (70,563,736) (2,408,776,608)
Net 202,253,392 88,006,295 3,421,634 110,825,463
UDC
1
(349,828) (151,345) (6,076) (192,407)
Total -
Billed $12,512,853,616 $5,685,014,240 $193,635,428 $6,634,203,948
Collected (12,011,396,719) (5,467,734,546) (184,732,406) (6,358,929,767)
UDC (349,828) (151,345) (6,076) (192,407)
Net
$501,107,069 $217,128,349 $8,896,946 $275,081,774
Aging -
Current $418,112,159 $180,888,729 $7,262,643 $229,960,787
61 Days to 2 Years
2
15,592,652 6,445,418 632,190 8,515,044
Over 2 Years 67,402,257 29,794,201 1,002,112 36,605,944
Total
3
$501,107,068 $217,128,348 $8,896,945 $275,081,775
1. UDC applied to CY18.
2. Pharmacy debt not delinquent until 70 days. 70-day A/R aging bucket not available; 61-day aging used instead.
3. 3QCY2018 Estimate added to Billings to reconcile with A/R: $117,137,000 MERHCF; $95,841,000 DHP & Non-DoD.
TRICARE has a waiver dated September 23, 1996, 10 USC 1079a, Champus: Treatment of Refunds and Other
Amounts Collected that states:
“All refunds and other amounts collected in the administration of the Civilian Health and Medical Program of the
Uniformed Services shall be credited to the appropriation available for that program for the fiscal year in which the
refund or amount is collected.”
Thus TRICARE records all Collections/Refunds into the current year and decreases budgetary disbursements for the
current year. The refunds collected are not treated as offsetting collections.
The DHA in FY 2018 continued to aggressively collect pharmacy refunds for both the Standard and Additional
Discount Programs. Through the concerted efforts of CRM, POD, HCDA, and OGC, DHA collected 98.9% of the
delinquent debt from 1st Quarter Calendar Year (CY) 2008 through 2nd Quarter CY 2017. All unpaid debts for these
quarters have been referred to the OGC’s Claims Collections Section and/or to the Department of the Treasury for
further collection activity.
The percent collected for 3rd Quarter CY 2017 through 1st Quarter CY 2018 is 97.8% with payments due for 2nd
Quarter CY 2018 in November 2018.

Management’s Discussion and Analysis
19
(Sources: PDW Reconned Cases Status 9.30.18 for 1QCY2015 to 2QCY2018 & DHA AR Activity 30-SEP-2018 for
1QCY2008 to 4QCY2014)
Forward Plans
The MHS Quadruple Aim is to increase readiness through better health, better care, and lower costs. The Quadruple
Aim serves as the strategic framework of the MHS, and in achieving this strategic framework, the DHA has adopted the
following three key goals:
Fortify our relationship with the Services
Strengthen our role as a Combat Support Agency
Optimize DHA operations
In response to the NDAA of FY 2017, the DHA continues to find efficiencies through consolidation of health care
plans, and integration of the direct health care facilities into the organization. The DHA has developed an
implementation plan based on the direction from Congress that will significantly alter the organizational structure of the
direct care facilities, enhancing coordination or healthcare activities for better patient care and improved cost
efficiencies. This plan will be effective 1 October 2018, and be fully implemented in FY 2020.
The majority of the impact of the changes will occur in the Military Treatment Facilities. As the centerpiece of the
Military Health System, the Private Sector Care contracts will continue to support those facilities as this transition
occurs. The changes directed by NDAA 2017, Section 702 are not expected to have a significant impact on the Private
Sector Care program.
The DHA Mission Statement is as follows:
The DHA, a Combat Support Agency, lead the MHS integrated system of readiness and health to deliver the Quadruple
Aim: increased readiness, better health, better care, and lower cost. DHA Director Priorities to align with the DHA
Mission are:
Empower and Care for Our People
Optimize Operations across the Military Health System
Co-create Optional Outcomes for Health, Well-being and Readiness
Deliver solutions to Combatant Commands
The DHA plan to accomplish the changes associated with NDAA 2017, Section 701, includes the key elements of the
mission statement above.
VI Limitations of the Financial Statements
The principal financial statements are prepared to report the financial position and results of operations of CRM,
pursuant to the requirements of 31 U.S.C. 3515(b). The statements are prepared from the books and records of Federal
entities in accordance with Federal Generally Accepted Accounting Principles (GAAP) and the formats prescribed by
OMB. Reports used to monitor and control budgetary resources are prepared from the same books and records. The
financial statements should be read with the realization they are for a component of the U.S. Government.
20
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
PRINCIPAL STATEMENTS

___________________________________________________Principal Statements
The accompanying notes are an integral part of these statements
21
Department of Defense
Defense Health Agency
Contract Resource Management
BALANCE SHEETS
As of September 30, 2018 and 2017
($ In Thousands)
2018 2017
Assets
Intragovernmental:
Fund Balance with Treasury (Note 2) $ 1,393,187 $ 1,675,116
Accounts Receivable (Note 3) 49,816 43,572
Total Intragovernmental 1,443,003 1,718,688
Cash and Other Monetary Assets (Note 4) 2,236 19
Accounts Receivable, Net 398,913 296,622
Total Assets
$ 1,844,152 $ 2,015,329
Liabilities
Intragovernmental:
Accounts Payable (Notes 5 and 6) $ 66,337 $ 74,194
Total Intragovernmental 66,337 74,194
Accounts Payable (Notes 5 and 6) 425,761 266,086
Military Retirement and Other Federal
Employment Benefits (Notes 5 and 9) 179,548,375 184,901,446
Other (Notes 5 and 7) 2,236 19
Total Liabilities
$ 180,042,709 $ 185,241,745
Commitments and Contingencies (Note 8)
Net Position
Unexpended Appropriations - Other Funds $ 950,905 $ 1,378,408
Cumulative Results of Operations - Other Funds (179,149,462) (184,604,824)
Total Net Position $ (178,198,557) $ (183,226,416)
Total Liabilities and Net Position
$ 1,844,152 $ 2,015,329
___________________________________________________Principal Statements
The accompanying notes are an integral part of these statements
22
Department of Defense
Defense Health Agency
Contract Resource Management
STATEMENTS OF NET COST
For the Years Ended September 30, 2018 and 2017
($ In Thousands)
2018 2017
Program Costs
Gross Costs (Note 10)
Operations, Readiness & Support $ 15,740,129 $ 15,651,278
Actuarial Non Assumption Costs (3,381,259) (689,143)
Less: Earned Revenue (1,253,893) (997,367)
Net Program Costs $ 11,104,977 $ 13,964,768
Gain/(Loss) from Actuarial Assumption Changes
for Military Retirement Benefits (Note 9) (1,830,406) 8,967,093
Net Program Costs Including Assumption Changes $ 9,274,571 $ 22,931,861
Net Cost of Operations
$ 9,274,571 $ 22,931,861
___________________________________________________Principal Statements
The accompanying notes are an integral part of these statements
23
Department of Defense
Defense Health Agency
Contract Resource Management
STATEMENTS OF CHANGES IN NET POSITION
For the Years Ended September 30, 2018 and 2017
($ In Thousands)
2018 2017
Unexpended Appropriations:
Beginning Balance $ 1,378,408 $ 1,136,900
Budgetary Financing Sources:
Appropriations received 14,380,099 15,006,527
Appropriations transferred-in/out (4,409) (55,000)
Other adjustments (rescissions, etc) (73,260) (120,576)
Appropriations used (14,729,933) (14,589,443)
Total Budgetary Financing Sources (427,503) 241,508
Total Unexpended Appropriations 950,905 1,378,408
Cumulative Results of Operations:
Beginning Balance (184,604,824) (176,262,406)
Budgetary Financing Sources:
Appropriations used 14,729,933 14,589,443
Transfers-in/out without reimbursement 0 0
Other 0 0
Total Financing Sources 14,729,933 14,589,443
Net Cost of Operations 9,274,571 22,931,861
Net Change 5,455,362 (8,342,418)
Cumulative Results of Operations
(179,149,462) (184,604,824)
Net Position
$ (178,198,557) $ (183,226,416)

___________________________________________________Principal Statements
The accompanying notes are an integral part of these statements
24
Department of Defense
Defense Health Agency
Contract Resource Management
STATEMENTS OF BUDGETARY RESOURCES
For the Years Ended September 30, 2018 and 2017
($ In Thousands)
2018 2017
Budgetary Resources
Unobligated balance from prior year budget authority, net $ 888,255 $ 395,340
Appropriations (discretionary and mandatory) 14,380,099 15,006,527
Spending authority from offsetting collections (discretionary
and mandatory) 1,236,715 1,003,632
Total Budgetary Resources
$ 16,505,069 $ 16,405,499
Status of Budgetary Resources
New obligations and upward adjustments (total) $ 16,035,766 $ 16,039,124
Unobligated balance, end of year
Unexpired unobligated balance, end of year 35,398 111,113
Expired unobligated balance, end of year 433,905 255,262
Unobligated balance, end of year (total) 469,303 366,375
Total Budgetary Resources
$ 16,505,069 $ 16,405,499
Outlays, Net
Outlays, net (total) (discretionary and mandatory) $ 14,584,358 $ 14,543,036
Agency Outlays, Net (discretionary and mandatory)
$ 14,584,358 $ 14,543,036
25
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
NOTES TO THE PRINCIPAL STATEMENTS

__________________________________________Notes to the Principal Statements
26
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
NOTES TO THE PRINCIPAL STATEMENTS
FOR THE YEARS ENDED SEPTEMBER 30, 2018 AND 2017
NOTE 1. SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
A. Mission of the Reporting Entity. The DHA is a DoD agency of the Under Secretary of Defense for Personnel and
Readiness and operates under the authority, direction, and control of the Assistant Secretary of Defense for Health
Affairs. The DHA has as one of its missions operational oversight of the MHS, including the direct care system
(military hospitals), the private sector care system, and management of MERHCF for those beneficiaries dual-
eligible for both Medicare and TRICARE.
TRICARE's primary mission is to enhance the DoD and our nation’s security by providing health care support for
the full range of military operations and sustaining the health of all those entrusted to our care, including active duty
personnel, military retirees, certain members of the Reserve Component, family members, widows, survivors, ex-
spouses, and other eligible members.
TRICARE’s vision is to be a world-class health care system that supports the military mission by fostering,
protecting, sustaining and restoring health. TRICARE’s vision:
To be the provider of premier care for our warriors and their families
To be an integrated team ready to go in harm’s way to meet our nation’s challenges at home or
abroad
To be a leader in health education training, research, and technology
To be a bridge to peace through humanitarian support
To be a nationally recognized leader in prevention and health promotion
The CRM office is responsible for the accounting and financial support and financial reporting for TRICARE’s
centrally funded private sector care programs. It draws funds from MERHCF to pay TRICARE for Life and
TRICARE Pharmacy private sector costs. The CRM is also responsible for reimbursable financial transactions
involving non-DoD services to the National Guard and Reserve Forces for private sector health care and for
reimbursable financial transactions involving medical services such as those provided by the Centers for Medicare &
Medicaid Services, related to private sector health care.
B. Basis of Presentation. These financial statements have been prepared to report the financial position and results
of operations of CRM, as required by the Chief Financial Officers Act of 1990, expanded by the Government
Management Reform Act of 1994, and other appropriate legislation. The financial statements have been prepared
from the books and records of CRM in accordance with, and to the extent possible, U.S. generally accepted
accounting principles (U.S. GAAP) promulgated by the Federal Accounting Standards Advisory Board; the OMB
Circular No. A-136, “Financial Reporting Requirements”; and the DoD, Financial Management Regulation (FMR).
The accompanying financial statements account for all resources for which CRM is responsible unless otherwise
noted.
On September 30, 2013, DoD Directive Number 5136.13 disestablished the TRICARE Management Activity
(TMA) and all TMA functions were transferred to DHA. TMA is now DHA with components including CRM,
USUHS and DHA-Comptroller (DHA-C) (formerly Financial Operations Division (FOD)). Any reference in law,
rule, regulation, or issuance to TMA will be deemed to be a reference to DHA, unless otherwise specified by the
Secretary of Defense.
The CRM is able to fully implement all elements of U.S. GAAP and the OMB Circular No. A-136. The CRM has
implemented an Oracle Based Federal Financial system.
__________________________________________Notes to the Principal Statements
27
C. Use of Estimates. The CRM’s management makes assumptions and reasonable estimates in the preparations of
financial statements based on current conditions which may affect the reported amounts. Actual results could differ
materially from the estimated amounts. Significant estimates include such items as accounts receivable, incurred but
not reported (IBNR) liabilities, and unfunded actuarial liabilities.
D. Appropriations and Funds. The CRM receives appropriations and funds as general, working capital (revolving),
trust, special funds, and deposit funds. The CRM uses these appropriations and funds to execute its missions and
subsequently report on resource usage.
General funds are used for financial transactions funded by congressional appropriations, including personnel,
operation and maintenance, research and development, procurement, and military construction.
Deposit funds are used to record amounts held temporarily until paid to the appropriate government or public entity.
They are not CRM funds, and as such, are not available for CRM’s operations. The CRM is acting as an agent or a
custodian for funds awaiting distribution.
For FY 2017, the Consolidated Appropriations Act, 2017, Public Law No. 115-31, became law May 5, 2017,
providing DoD funding for FY 2017, replacing the Continuing Resolution in effect since the beginning of the fiscal
year.
For FY 2018, the Consolidated Appropriations Act, 2018, Public Law No. 115-141, became law March 23, 2018,
providing DoD funding for FY 2018, replacing the Continuing Resolution in effect since the beginning of the fiscal
year.
E. Basis of Accounting. The financial transactions are recorded on a proprietary accrual and a budgetary basis of
accounting. Under the accrual basis, revenues are recognized when earned and expenses are recognized when
incurred, without regard to the timing of receipt or payment of cash. Whereas, under the budgetary basis the legal
commitment or obligation of funds is recognized in advance of the proprietary accruals and compliance with legal
requirements and controls over the use Federal funds.
The CRM financial statements and supporting trial balances are compiled from the underlying financial data and
trial balances of CRM's feeder systems. The underlying data is largely derived from budgetary transactions
(obligations, disbursements, and collections), from nonfinancial feeder systems, and accruals made for major items
such as accounts payable and actuarial liabilities.
F. Revenues and Other Financing Sources. The CRM receives congressional appropriations as financing sources for
general funds that expire annually, on a multi-year basis, or do not expire. When authorized by legislation, these
appropriations are supplemented by revenues generated by sales of goods or services. The CRM recognizes revenue
as a result of costs incurred for goods and services provided to other federal agencies and the public. Full cost
pricing is CRM’s standard policy for services provided as required by OMB Circular A-25, “User Charges”. In
some instances, revenue is recognized when bills are issued.
The CRM does not include nonmonetary support provided by U.S. allies for common defense and mutual security in
amounts reported in the Statement of Net Cost and the Note 13, Reconciliation of Net Cost of Operations to Budget.
The U.S. has cost sharing agreements with countries having a mutual or reciprocal defense agreement, where U.S.
troops are stationed, or where the U.S. Fleet is in a port.
In accordance with Statement of Federal Financial Accounting Standards (SFFAS) Number 7 “Accounting for
Revenue and Other Financing Sources and Concepts for Reconciling Budgetary and Financial Accounting”, CRM
recognizes nonexchange revenue when there is a specifically identifiable, legally enforceable claim to the cash or
other assets of another party that will not directly receive value in return.
G. Recognition of Expenses. For financial reporting purposes, DoD policy requires the recognition of operating
expenses in the period incurred. Estimates are made for major items such as IBNR liabilities and unfunded actuarial
liabilities. Accrual adjustments are made for major items such as accounts payable.
__________________________________________Notes to the Principal Statements
28
H. Accounting for Intragovernmental Activities. The Treasury Financial Manual Part 2 – Chapter 4700, Agency
Reporting Requirements for the Financial Report of the United States Government, provides guidance for reporting
and reconciling intragovernmental balances. Accounting standards require an entity to eliminate intra-entity activity
and balances from consolidated financial statements to prevent overstatement for business with itself. Generally,
seller entities within the DoD provide summary seller-side balances for revenue, accounts receivable, and unearned
revenue to the buyer-side internal accounting offices. The DoD is implementing replacement systems and a standard
financial information structure that will incorporate the necessary elements to enable DoD to correctly report,
reconcile, and eliminate intragovernmental balances.
Imputed financing represents the costs paid on behalf of the CRM by another Federal entity for business-type
activity. The DHA-C recognizes CRM’s imputed costs for (1) employee pension, post-retirement health, and life
insurance benefits; (2) post-employment benefits for terminated and inactive employees to include unemployment
and workers compensation under the Federal Employees’ Compensation Act; and (3) losses in litigation
proceedings. Consistent with the implementation of SSFAS No. 55, “Amending Inter-Entity Cost Provisions”,
certain unreimbursed inter-entity costs of goods and services other than those identified in the preceding are not
included in the financial statements.
The DoD’s proportionate share of public debt and related expenses of the Federal Government is not included. The
Federal Government does not apportion debt and its related costs to federal agencies. The DoD’s financial
statements do not report any public debt, interest, or source of public financing, whether from issuance of debt or tax
revenues.
I. Funds with the U.S. Treasury. The CRM’s monetary resources of collections and disbursements are maintained in
U.S. Treasury accounts. The CRM’s cash collections, disbursements, and adjustments are processed by CRM
through the U.S. Treasury. The CRM prepares monthly reports to the U.S. Treasury on checks issued, electronic
fund transfers, interagency transfers, and deposits.
In addition, Defense Finance and Accounting Service (DFAS) and the U.S. Army Corps of Engineers (USACE)
Finance Center submit reports to the U.S. Treasury by appropriation on interagency transfers, collections received,
and disbursements issued. The U.S. Treasury records these transactions to the applicable FBWT account.
The CRM has been authorized direct access to U.S. Treasury systems to make payments and collections due to the
size and nature of their Purchased-Care programs. U.S. Treasury expenditure reporting is combined with DoD
expenditure reporting for CRM by DFAS-IN.
J. Cash and Other Monetary Assets. Cash is the total of cash resources under the control of CRM including coin,
paper currency, negotiable instruments, and amounts held for deposit in banks and other financial institutions.
Foreign currency consists of the total U.S. dollar equivalent of both purchased and nonpurchased foreign currencies
held in foreign currency fund accounts. Foreign currency is valued using the U.S. Treasury prevailing rate of
exchange.
The majority of cash and other monetary assets is classified as “nonentity” and is restricted. Cash and other
monetary assets reported consist of undeposited collections received by CRM before month-end but after the U.S.
Treasury month-end cutoff. A corresponding liability is recorded because CRM is not entitled to the funds until
deposited with the U.S. Treasury.
The CRM conducts a portion of its operations overseas. Congress established a special account to handle the gains
and losses from foreign currency transactions for five general fund appropriations: (1) operations and maintenance;
(2) military personnel; (3) military construction; (4) family housing operations and maintenance; and (5) family
housing construction. The gains and losses are calculated as t
he variance between the exchange rate current at the
date of payment and a budget rate established at the beginning of each fiscal year. Monthly an invoice/payment is
submitted to CRM for processing. Foreign currency fluctuations related to other appropriations require adjustments
to the original obligation amount at the time of payment. The CRM does separately identify currency fluctuation
transactions.
__________________________________________Notes to the Principal Statements
29
K. Accounts Receivable. Accounts receivable from other federal entities or the public include accounts receivable,
claims receivable, and refunds receivable. Allowances for uncollectible accounts due from the public are based
upon factors such as: aging of accounts receivable, debtor’s ability to pay, and payment history. The CRM does not
recognize an allowance for estimated uncollectible amounts from other federal agencies as receivables from other
federal agencies are considered to be inherently collectible. Claims for accounts receivable from other federal
agencies are to be resolved between the agencies in accordance with the Intragovernmental Business Rules
published in the Treasury Financial Manual.
Since the beginning of the FCP Program, outpatient pharmaceuticals purchased by DoD through medical treatment
facility pharmacies have been subject to FCPs, as have those under the TMOP program. The DHA implemented
FCPs for the TRICARE Retail Pharmacy program in compliance with the NDAA for Fiscal Year 2008, §703. The
Final Rule was published March 17, 2009 and was updated October 15, 2010. The DHA applied this rule to all
retail prescriptions filled subsequent to January 28, 2008 unless the DHA (formerly TMA) granted a waiver to a
particular manufacturer. Compliance is mandatory and the advantage to the manufacturers is that their drugs will be
included on the DoD Uniform Formulary (list of available prescription drugs). The DHA records accounts
receivable upon receipt of the calculation from the TRICARE Pharmacy Operations Directorate and posts
collections from the manufacturers to the fiscal year of receipt pursuant to Title 10, U.S.C. §1079a.
L. Contingencies and Other Liabilities. The SFFAS No. 5, “Accounting for Liabilities of the Federal Government,”
as amended by SFFAS No. 12, “Recognition of Contingent Liabilities Arising from Litigation”, defines a
contingency as an existing condition, situation, or set of circumstances that involves an uncertainty as to possible
gain or loss. The uncertainty will be resolved when one or more future events occur or fail to occur. The CRM
recognizes contingent liabilities when past events or exchange transactions occur, a future loss is probable, and the
loss amount can be reasonably estimated.
Financial statement reporting is limited to disclosure when conditions for liability recognition do not exist but there
is at least a reasonable possibility of incurring a loss or additional losses. The CRM’s risk of loss and resultant
contingent liabilities arise from pending or threatened litigation or claims and assessments due to events such as
medical malpractice; property or environmental damages; and contract disputes.
M. Net Position. Net position consists of unexpended appropriations and cumulative results of operations.
N. Undistributed Disbursements and Collections. Undistributed disbursements and collections represent the
difference between disbursements and collections matched at the transaction level to specific obligations, payables,
or receivables in the source systems and those reported by the U.S. Treasury. Supported disbursements and
collections have corroborating documentation for the summary level adjustments made to accounts payable and
receivable. Unsupported disbursements and collections do not have supporting documentation for the transactions
and most likely would not meet audit scrutiny. However, both supported and unsupported adjustments may have
been made to the CRM accounts payable and receivable trial balances prior to validating underlying transactions.
O. Military Retirement and Other Federal Employment Benefits. The Department applies SFFAS No. 33,
"Pensions, Other Retirement Benefits, and Other Postemployment Benefits: Reporting the Gains and Losses from
Changes in Assumptions and Selecting Discount Rates and Valuation Dates", in selecting the discount rate and
valuation date used in estimating actuarial liabilities. In addition, gains and losses from changes in long-term
assumptions used to estimate the actuarial liability are presented separately on the Statement of Net Cost. Refer to
Note 9, Military Retirement and Other Federal Employment Benefits and Note 10, General Disclosures Related to
the Statement of Net Cost, for additional information.
P. Reclassifications. Certain amounts in the prior year's SBR have been reclassified to conform to the current year's
presentation. These reclassifications had no effect on the previously reported SBR.

__________________________________________Notes to the Principal Statements
30
NOTE 2. FUND BALANCE WITH TREASURY
($ In Thousands) 2018 2017
Status of Funds Balance with Treasury
Unobligated Balance
Unobligated Balance - Available $ 35,398 $ 111,113
Unobligated Balance - Unavailable 433,905 255,262
Obligated Balance not yet Disbursed 990,691 1,386,480
Non-Budgetary FBWT (66,807) (77,739)
Total $ 1,393,187 $ 1,675,116
The Treasury records cash receipts and disbursements on CRM’s behalf and are available only for the purposes for
which the funds were appropriated. The CRM’s fund balances with treasury consists of appropriation accounts.
The Status of FBWT reflects the budgetary resources to support FBWT and is a reconciliation between budgetary
and proprietary accounts. It primarily consists of unobligated and obligated balances. The balances reflect the
budgetary authority remaining for disbursement against current or future obligations.
Unobligated Balance is classified as available or unavailable and represents the cumulative amount of budgetary
authority that has not been set aside to cover future obligations. Certain unobligated balances are restricted for
future use and are not apportioned for current use.
Obligated Balance not yet Disbursed represents funds obligated for goods and services but not paid.
Non-FBWT Budgetary Accounts reduces the Status of FBWT, such as reimbursable authority, comprised of
reimbursable accounts receivable of $49.8 million, and reimbursable undelivered orders of $17.0 million.
__________________________________________Notes to the Principal Statements
31
NOTE 3. ACCOUNTS RECEIVABLE, NET
($ In Thousands) 2018
Allowance for Accounts
Gross Estimated Receivable,
Amount Due Uncollectibles Net
Intragovernmental Receivables $ 49,816 $ N/A $ 49,816
Nonfederal Receivables (From the Public) 428,869 (29,956) 398,913
Total Accounts Receivable $ 478,685 $ (29,956) $ 448,729
2017
Allowance for Accounts
Gross Estimated Receivable,
Amount Due Uncollectibles Net
Intragovernmental Receivables $ 43,572 $ N/A $ 43,572
Nonfederal Receivables (From the Public) 324,106 (27,484) 296,622
Total Accounts Receivable $ 367,678 $ (27,484) $ 340,194
Accounts Receivable (A/R) represent CRM's claim for payment from other entities. The CRM only recognizes an
allowance for uncollectible amounts from the public. The method used to calculate the percentage for bad debt
allowance on the uncollected A/R amounts is determined by taking a 12 month average of the A/R balance against
the 12 month average on the Write Off balance per each Receivable category. The data from the prior 12 months is
used to calculate the percentages for the allowance. The CRM has one specific A/R category that follows a different
percentage calculation rule, the "Suspended Pharmacy" category. Per a DHA Program Integrity directive that
prevents CRM’s Pharmacy contractor from pursuing collection action against Suspended Pharmacies while under
investigation, CRM uses a 100% Allowance methodology for calculating the debt against the A/R balance. Claims
with other federal agencies are resolved in accordance with the Intragovernmental Business Rules.
As of September 30, 2018, the total net receivables recorded for SDP and the ADP were $188.6 million. The SDP
resulted from the implementation of the Federal Ceiling Program for the TRICARE Retail Pharmacy Refunds
Program as required by the FY 2008 NDAA, Section 703. The ADP resulted from voluntary agreements between
TRICARE and the pharmaceutical manufacturers providing additional discounts above the SDP.
NOTE 4. CASH AND OTHER MONETARY ASSETS
($ In Thousands) 2018 2017
Cash $ 2,236 $ 19
Total Cash and Other Monetary Assets $ 2,236 $ 19
Cash and other monetary assets reported consist of undeposited collections received by CRM before month-end but
after the U.S. Treasury month-end cutoff. A corresponding liability is recorded because CRM is not entitled to the
funds until deposited with the U.S. Treasury.
__________________________________________Notes to the Principal Statements
32
NOTE 5. LIABILITIES NOT COVERED BY BUDGETARY RESOURCES
($ In Thousands) 2018 2017
Military Retirement and Other Federal Employment
Benefits $ 179,548,375 $ 184,901,446
Total Liabilities Not Covered by Budgetary Resources $ 179,548,375 $ 184,901,446
Total Liabilities Covered by Budgetary Resources 494,334 340,299
Total Liabilities $ 180,042,709 $ 185,241,745
The CRM has two liabilities not covered by budgetary resources. Military Retirement and Other Federal
Employment Benefits consists of various employee actuarial liabilities not due and payable during the current fiscal
year. These liabilities primarily consist of $179.5 billion in health benefit liabilities, with $178.1 billion in actuarial
liabilities for future health benefits and $1.4 billion in IBNR health benefits. The DHA, as stated in the Senate
Report No. 95-1264 on the Department of Defense Appropriation Bill, FY 1979, does not obligate or fund health
care claims until the receipt of an adjudicated claim. Consequently, no funding or obligations occur for these
liabilities until health care is rendered and the CRM is in receipt of an adjudicated claim. Refer to Note 9, Military
Retirement and Other Federal Employment Benefits, for additional details.
NOTE 6. ACCOUNTS PAYABLE
($ In Thousands) 2018
Interest, Penalties
Accounts
and
Administrative
Payable Fees Total
Intragovernmental Payables $ 66,337 $ N/A $ 66,337
Nonfederal Payables (To the Public) 425,761 0 425,761
Total Accounts Payable $ 492,098 $ 0 $ 492,098
2017
Interest, Penalties
Accounts
and
Administrative
Payable Fees Total
Intragovernmental Payables $ 74,194 $ N/A $ 74,194
Nonfederal Payables (To the Public) 266,086 0 266,086
Total Accounts Payable $ 340,280 $ 0 $ 340,280
Accounts Payable include amounts owed to Federal and non-Federal entities for goods and services received by
CRM.
__________________________________________Notes to the Principal Statements
33
NOTE 7. OTHER LIABILITIES
($ In Thousands) 2018 2017
Nonfederal Other Liabilities 2,236 19
Total Other Liabilities $ 2,236 $ 19
Total Nonfederal Other Liabilities consist of undeposited collections received by CRM before month-end but after
the U.S. Treasury month-end cutoff. A corresponding liability is recorded because CRM is not entitled to the funds
until deposited with the U.S. Treasury. All amounts presented herein are considered current liabilities.
NOTE 8. COMMITMENTS AND CONTINGENCIES
The CRM is a party in various administrative proceedings and legal actions related to claims for contractual bid
processes. The CRM is unaware of any contingent liabilities for legal actions.
The CRM accrues contingent liabilities for legal actions where the OGC considers an adverse decision probable and
the amount of loss measurable. In the event of an adverse judgment against the Government, some of the liabilities
may be payable from the U.S. Treasury Judgment Fund. The CRM records contingent liabilities in Note 7, Other
Liabilities.
Amounts disclosed for litigation claims and assessments are fully supportable and agree with the DHA’s legal
representation letters and management summary schedule.
The CRM will disclose an estimate of obligations related to cancelled appropriations for which the CRM has a
contractual commitment for payment and amounts for contractual arrangements which may require future financial
obligations, when there are any.
The CRM will disclose amounts for potential future obligations such as contractual arrangements for fixed price
contracts with escalation, price redetermination, or incentive clauses; contracts authorizing variations in quantities;
and contracts where allowable interest may become payable based on contractor claims under the “Disputes” clause
contained in contracts, when there are any. Amounts disclosed will represent future potential liabilities and will not
include amounts already recognized as contingent liabilities in Note 7. Consideration will be given in disclosing the
difference between the maximum or ceiling amounts and those amounts recognized in Note 7 when it is reasonably
possible the maximum amount may be paid.
There are three cases or claims pending with the DHA meeting the threshold guidance of an amount being claimed
at or exceeding $3.6 million or multiple cases or claims arising out of a single action, incident or factual
circumstances where, in the aggregate, the amount claimed is or exceeds $13.1 million.
Ingham Regional Medical Center v. United States (Court of Federal Claims). Class action, but not certified,
alleging DoD, in reaching a resolution of hospital outpatient radiology claims, entered into contracts with the named
plaintiffs. Plaintiffs’ First Amended Complaint was filed on November 17, 2014. The Amended Complaint alleges
breach of express contract, breach of implied contract, mutual mistake, breach of the covenant of good faith and fair
dealing, and violations of a statutory mandate under the TRICARE statute. The suit alleges 5,200 hospitals were
underpaid for outpatient procedures. On March 22, 2016, the Court of Federal Claims issued its decision granting
the Government’s Motion to Dismiss Plaintiffs’ Amended Complaint. Plaintiffs appealed to the Court of Appeals
for the Federal Circuit. On November 3, 2017, the Court of Appeals reversed the dismissal of Ingham’s breach of
contract claim and remanded the case to the trial court for further proceedings on that claim. On March 20, 2018,
the government filed its Answer to the First Amended Complaint. The parties are proceeding with discovery.
__________________________________________Notes to the Principal Statements
34
Central Rexall Drugs, Inc. v. Defense Health Agency Director, Raquel C. Bono (U.S. District Court, Eastern
District of Louisiana). Plaintiff seeks a Writ of Mandamus ordering the DHA Director to lift the claims payment
suspension and pay pending claims worth approximately $21 million. Plaintiff alleges the permissible length of
time the DHA may suspend claims payment expired and, therefore, the DHA is obligated to pay the claims. The
DHA contends it has authority to continue the suspension. The DOJ filed a Motion to Dismiss on 7 July 2017, and
the Court’s decision is pending.
Smart Pharmacy, Inc., et al. v. Vice Admiral Raquel C. Bono, Director, Defense Health Agency (U.S. District
Court, District of Florida). Plaintiffs are compound pharmacies. In response to revelations compound pharmacies
had been submitting fraudulent claims to the Government, the DHA suspended claims processing payments for
several compound pharmacies, including Plaintiffs, pending an investigation. Plaintiffs seek declaratory judgments
prohibiting the DHA from suspending claim processing and payments, from collecting claim clawbacks, and that the
HHS OIG is violating federal laws and regulations. Plaintiffs allege the DHA improperly suspended claims
processing, while the DHA contends it has authority to suspend claims processing under these circumstances.
Plaintiffs filed the Complaint on April 19, 2018, and mailed the Complaint and A Notice of a Lawsuit and Request
to Waive Service of a Summons to Vice Admiral Bono on April 27, 2018. The Government is reviewing the
Complaint’s allegations and will decide whether to file an Answer or dispositive motion(s). Based on the allegations
in the Complaint, the amount sought is at least $4 million.
NOTE 9. MILITARY RETIREMENT AND OTHER FEDERAL EMPLOYMENT BENEFITS
($ In Thousands) 2018
Less Assets
Available to Unfunded
Liabilities Pay Benefits Liabilities
Military Pre Medicare-Eligible Retiree
Health Benefits $ 178,118,419 $ 0 $ 178,118,419
Other 1,429,956 0 1,429,956
Total Military Retirement and Other Federal
Employment Benefits $ 179,548,375 $ 0 $ 179,548,375
2017
Less Assets
Available to Unfunded
Liabilities Pay Benefits Liabilities
Military Pre Medicare-Eligible Retiree
Health Benefits $ 183,330,084 $ 0 $ 183,330,084
Other 1,571,362 0 1,571,362
Total Military Retirement and Other Federal
Employment Benefits $ 184,901,446 $ 0 $ 184,901,446
Information Related to Military Retirement and Other Federal Employment Benefits
The DoD Office of the Actuary (DoD OACT) calculates the actuarial liability at the end of each fiscal year using the
current active and retired population, plus assumptions about future demographic and economic conditions.
The schedules above reflect two distinct types of liabilities related to Military Retirement and Other Federal
Employment Benefits. The line entitled “Military Pre Medicare-Eligible Retiree Health Benefits” represents the

__________________________________________Notes to the Principal Statements
35
actuarial (or accrued) liability for future health care benefits provided to non-Medicare-eligible retired beneficiaries
that are not yet incurred. The line entitled “Other” includes the IBNR reserve, which is an estimate of benefits
already incurred but not yet reported to DoD for all DHP beneficiaries (excluding those from the retiree population
who are Medicare-eligible).
Effective FY 2010, DHA implemented requirements of SFFAS No. 33, which directs that the discount rate,
underlying inflation rate, and other economic assumptions be consistent with one another. A change in the discount
rate may cause other assumptions to change as well. For the September 30, 2018, financial statement valuation, the
application of SFFAS No. 33 required DoD OACT to set the long-term inflation (CPI) to be consistent with the
underlying Treasury spot rates used in the valuation.
The DHA actuarial liability is adjusted at the end of each fiscal year. The 4th Quarter, FY 2018 balance represents
the September 30, 2018 amount that is effective through 3rd Quarter of FY 2019.
Actuarial Cost Method
As prescribed by SFFAS No. 5, the valuation of DHA Military Retirement Health Benefits is performed using the
Aggregate Entry Age Normal (AEAN) cost method. AEAN is a method whereby projected retiree medical plan
costs are spread over the projected service of a new entrant cohort.
Assumptions
For the FY 2018 financial statement valuation, the long-term assumptions include a 3.6% discount rate and medical
trend rates that were developed using a 1.5% inflation assumption. Note that the term ’discount rate’ refers to the
interest rate used to discount cash flows. The terms ‘interest rate’ and ‘discount rate’ are often used interchangeably
in this context.
For the FY 2017 financial statement valuation, the long-term assumptions included a 3.8% discount rate and medical
trend rates that were developed using a 1.7% inflation assumption.
The change in the long-term assumptions is due to the application of SFFAS No. 33. This applicable financial
statement standard is discussed further below. Other assumptions used to calculate the actuarial liabilities, such as
mortality and retirement rates, were based on a blend of actual experience and future expectations. Because of
reporting deadlines, and as permitted by SFFAS No. 33, the current year actuarial liability is rolled forward from the
prior year valuation results using accepted actuarial methods.
In calculating the FY 2018 ”rolled-forward” actuarial liability, the following assumptions were used:
Discount Rate 3.6%
Inflation 1.5%
Medical Trend (Non-Medicare)
FY 2017 - FY 2018 Ultimate Rate 2042
Purchased Care Inpatient 1.95% 4.00%
Purchased Care Outpatient 3.30% 4.00%
Purchased Care Prescription Drugs 3.28% 4.00%
Purchased Care USFHP 3.95% 4.00%
After a 25 year select period, an ultimate trend rate is assumed for all future projection years.
__________________________________________Notes to the Principal Statements
36
Military Pre Medicare-Eligible Retiree Health Benefits
($ In Thousands) 2018 2017
Beginning Actuarial Liability $ 183,330,084 $ 175,052,134
Plus Expenses:
Normal Cost 7,125,531 6,631,465
Interest Cost 7,082,209 7,107,094
Plan Amendments (2,709,849) 0
Experience Losses/(Gains) (6,638,932) (6,335,890)
Other Factors 0 1
Subtotal: Expenses Before Losses/(Gains) From
Actuarial Assumption Changes 4,858,959 7,402,670
Actuarial Losses/(Gains) Due To:
Changes In Trend Assumptions (3,861,486) 1,376,788
Changes In Assumptions Other Than Trend 2,031,080 7,590,305
Subtotal: Losses/(Gains) From Actuarial Assumption
Changes (1,830,406) 8,967,093
Total Expenses $ 3,028,553 $ 16,369,763
Less Benefit Outlays 8,240,218 8,091,813
Total Changes In Actuarial Liability $ (5,211,665) $ 8,277,950
Ending Actuarial Liability $ 178,118,419 $ 183,330,084
The DHA actuarial liability decreased $5.2 billion (2.8%). This resulted from the net effect of: an increase of $6.0
billion due to expected increases (interest cost plus normal cost less benefit outlays), a decrease of $1.8 billion due
to changes in key assumptions; a decrease of $2.7 billion due to a plan change; and a decrease of $6.6 billion due to
actual experience being different from what was assumed (demographic and claims data).
DoD complies with SFFAS No. 33, "Pensions, Other Retirement Benefits, and Other Postemployment Benefits:
Reporting the Gains and Losses from Changes in Assumptions and Selecting Discount Rates and Valuation Dates."
The standard requires the separate presentation of gains and losses from changes in long-term assumptions used to
estimate liabilities associated with pensions, other retirement and other postemployment benefits. SFFAS No. 33
also provides a standard for selecting the discount rate and valuation date used in estimating these liabilities. SFFAS
No. 33, as published on October 14, 2008, by the Federal Accounting Standards Advisory Board (FASAB) requires
the use of a yield curve based on marketable U.S. Treasury Securities to determine the discount rates used to
calculate actuarial liabilities for federal financial statements. Historical experience is the basis for expectations
about future trends in marketable U.S. Treasury securities.
The statement is effective for periods beginning after September 30, 2009, and applies to information provided in
general purpose federal financial statements. It does not affect statutory or other special-purpose reports such as
Pension or Other Retirement Benefit reports. SFFAS No. 33 requires a minimum of five periodic rates for the yield
curve input and consistency in the number of historical rates used from period to period. It permits the use of a
single average discount rate if the resulting present value is not materially different from what would be obtained
using the yield curve.
For the September 30, 2018 financial-statement valuation, DoD OACT determined a single equivalent discount rate
of 3.6% by using a 10-year average of quarterly zero coupon Treasury spot rates. These spot rates are based on the

__________________________________________Notes to the Principal Statements
37
U.S. Department of the Treasury – Office of Economic Policy’s 10-year Average Yield Curve for Treasury Nominal
Coupon Issues (TNC yield curve),which represents average rates from April 1, 2008 through March 31, 2018.
NOTE 10. GENERAL DISCLOSURES RELATED TO THE STATEMENT OF NET COST
($ In Thousands) 2018 2017
Gross Cost
Intragovernmental Cost $ 715,428 $ 802,645
Nonfederal Cost 11,643,442 14,159,490
Total Cost 12,358,870 14,962,135
Earned Revenue
Intragovernmental Revenue (576,170) (569,093)
Nonfederal Revenue (677,723) (428,274)
Total Revenue (1,253,893) (997,367)
Losses/(Gains) from Actuarial Assumption
Changes for Military Retirement Benefits (1,830,406) 8,967,093
TOTAL NET COST
$ 9,274,571 $ 22,931,861
The Statement of Net Cost (SNC) represents the net cost of programs and organizations of CRM that are supported
by appropriations or other means. The intent of the SNC is to provide gross and net cost information related to the
amount of output or outcome for a given program or organization administered by a responsible reporting entity.
The DoD’s current processes and systems capture costs based on appropriations groups as presented in the schedule
above. The lower level costs for major programs are not presented as required by the Government Performance and
Results Act. The DoD is in the process of reviewing available data and developing a cost reporting methodology as
required by SFFAS No. 4, “Managerial Cost Accounting Concepts and Standards for the Federal Government,” as
amended by SFFAS No. 55, “Amending Inter-Entity Cost Provisions.”
Effective Fiscal Year 2018, the Department has elected early implementation of SFFAS No. 55 which rescinds
SFFAS No. 30, “Inter-Entity Cost Implementation: Amending SFFAS No. 4, Managerial Cost Accounting
Standards and Concepts and Interpretation 6, Accounting for Imputed Intra-departmental Costs: An Interpretation
of SFFAS No. 4.”
The Department Military Retirement and post-employment costs are reported in accordance with SFFAS No. 33,
“Pensions, Other Retirement Benefits, and Other Postemployment Benefits: Reporting the Gains and Losses from
Changes in Assumptions and Selecting Discount Rates and Valuation Dates.” The standard requires the separate
presentation of gains and losses from changes in long-term assumptions used to estimate liabilities associated with
pensions, other retirement and other postemployment benefits on the SNC.
NOTE 11. DISCLOSURES RELATED TO THE STATEMENT OF CHANGES IN NET POSITION
Appropriations received decreased by $626.4 million (4%) due to the startup of the new T2017 Managed Care
Support Contract, which provided a significant reduction in costs. As of January 2018, CRM began receiving Prime
Enrollment Fees, which were previously kept by the contractor. These Enrollment Fees offset CRM’s expenditures,
lowering the appropriation required.
Program obligations decreased by $550.7 million primarily due to decreases in Managed Care Support Contracts of
$349.5 million, TMOP of $120.9 million, and Supplemental Health Care of $112.3 million, 106% of the decrease.

__________________________________________Notes to the Principal Statements
38
NOTE 12. DISCLOSURES RELATED TO THE STATEMENT OF BUDGETARY RESOURCES
($ In Thousands) 2018 2017
Intragovernmental Budgetary Resources Obligated for Undelivered Orders
Unpaid 14,745 48,524
Total Intragovernmental 14,745 48,524
Nonfederal Budgetary Resources Obligated for Undelivered Orders
Unpaid 483,847 997,678
Total Nonfederal 483,847 997,678
Net Amount of Budgetary Resources Obligated for Undelivered Orders
at the End of the Period $ 498,592 $ 1,046,202
Direct Obligations
Category A $ 14,578,066
Category B 200,783
Exempt from Apportionment 0
Total Direct Obligations 14,778,849
Reimbursable Obligations
Category A 1,256,917
Category B 0
Exempt from Apportionment 0
Total Reimbursable Obligations 1,256,917
Total Obligations $ 16,035,766
The CRM has no legal arrangements, other than time limits applied to obligational authority, affecting the use of
unobligated balances of budget authority. The CRM has not identified any material differences between amounts
reported on the Statement of Budgetary Resources (SBR) and the Standard Form (SF) 133, Report on Budget
Execution.
__________________________________________Notes to the Principal Statements
39
NOTE 13. RECONCILIATION OF NET COST OF OPERATIONS TO BUDGET
($ In Thousands) 2018 2017
Resources Used to Finance Activities:
Budgetary Resources Obligated:
Obligations Incurred $ 16,035,766 $ 16,039,124
Less: Spending authority from offsetting collections
and recoveries (-) (1,836,265) (1,260,716)
Net obligations 14,199,501 14,778,408
Other Resources:
Other (+/-) 0 0
Total resources used to finance activities 14,199,501 14,778,408
Resources Used to Finance Items Not Part of the Net Cost
of Operations:
Change in budgetary resources obligated for goods, services
and benefits ordered but not yet provided:
Undelivered Orders (-) 547,610 (195,231)
Unfilled Customer Orders (17,178) 6,266
Resources that fund expenses recognized in
prior periods (7,384,151) 0
Other resources or adjustments to net obligated resources
that do not affect Net Cost of Operations:
Other (+/-) 0 0
Total resources used to finance items not part of the Net Cost
of Operations (6,853,719) (188,965)
Total resources used to finance the Net Cost of Operations 7,345,782 14,589,443
Components of the Net Cost of Operations that will not
Require or Generate Resources in the Current Period:
Components Requiring or Generating Resources in
Future Period:
Other (+/-) 2,031,080 8,300,237
Components not Requiring or Generating Resources:
Other (+/-) (102,291) 42,181
Total components of Net Cost of Operations that will not
require or generate resources in the current period 1,928,789 8,342,418
Net Cost of Operations 9,274,571 22,931,861
Line 23, Components requiring or generating resources in future period, other, must be compared with and netted
against Line 13, resources that fund expenses recognized in prior periods, to determine the net change. The accounts
that support these line items include the change in the IBNR Liability and the Actuarial Liability. Refer to Note 9
for more specific information regarding these liabilities. Line 13 reflects a net change of $7.4 billion, comparing 4th
Quarter, FY 2018 to 4th Quarter, FY 2017. Line 23 reflects a net change of $6.3 billion, comparing 4th Quarter, FY
2018 to 4th Quarter, FY 2017. The net change equals $13.7 billion.
__________________________________________Notes to the Principal Statements
40
The balance in components not requiring or generating resources represents components of the net cost of operations
that will not require or generate resources in the current period. There is an overall decrease of $144.5 million due
to net changes in Accounts Receivable and Bad Debt Expense.
41
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
OTHER INFORMATION

42
EXHIBIT 1
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
SUMMARY OF FINANCIAL STATEMENT AUDIT AND MANAGEMENT ASSURANCES
SEPTEMBER 30, 2018
Agencies are required to provide certain assurances as to the status and effectiveness of the internal controls and
financial management systems that support the preparation of the financial statements. In the context of the CRM
Management’s Discussion and Analysis, DoD, and not CRM, represents the legislative definition of an Agency.
Beginning with FY 2006, as directed in OMB Circular A-123, Management’s Responsibility for Enterprise Risk
Management and Internal Control, Appendix A, Internal Control Over Financial Reporting, the 24 CFO Act
agencies (includes DoD), are required to provide a separate assessment of the effectiveness of the internal controls
over financial reporting as a subset of the overall FMFIA assurance statement. OUSD(C) issued guidelines to the
leadership of DoD Components, including CRM, as to how to support this DoD reporting requirement. CRM
management complied with the required guidelines and issued their Annual Statement of Assurance Required Under
the FMFIA, dated September 30, 2018.
As required by OMB A-136, Section II.4.4, the following summarizes CRM’s Financial Statement Audit and
Management Assurances:
Table 1. Summary of Financial Statement Audit
Audit Opinion Unmodified
Restatement No
Material Weaknesses Beginning
Balance
New Resolved Consolidated Ending
Balance
N/A
Total Material Weaknesses 0 0 0 0 0
Table 2. Summary of Management Assurances
Effectiveness of Internal Controls over Financial Reporting (FMFIA § 2)
Statement of Assurance Unmodified
Material Weaknesses Beginning
Balance
New Resolved Consolidated Reassessed Ending
Balance
Total Material Weaknesses 0 0 0 0 0 0

43
Effectiveness of Internal Controls over Operations (FMFIA § 2)
Statement of Assurance Unmodified
Material Weaknesses Beginning
Balance
New Resolved Consolidated Reassessed Ending
Balance
Total Material Weaknesses 0 0 0 0 0 0
Compliance with Section 803(a) of the Federal Financial Management Improvement Act (FFMIA)
Agency Auditor
Federal Financial Management Systems
Requirements
No lack of compliance noted No lack of compliance noted
Applicable Federal Accounting Standards No lack of compliance noted No lack of compliance noted
USSGL at Transaction Level No lack of compliance noted No lack of compliance noted
Conformance with Federal Financial Management System Requirements (FMFIA § 4)
Statement of Assurance Federal Systems conform to financial management systems requirements
Non-Conformances Beginning
Balance
New Resolved Consolidated Reassessed Ending
Balance
Total Non-Conformances 0 0 0 0 0 0

44
EXHIBIT 2
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
FY 2017-2018 RISK ASSESSMENT
MILITARY HEALTH BENEFITS PROGRAM
SEPTEMBER 30, 2018
PAYMENT INTEGRITY REPORTING FOR THE DEFENSE HEALTH AGENCY
Payment Integrity
The Federal Improper Payments Coordination Act of 2015 amended the Improper Payment Elimination and
Recovery Improvement Act of 2012 (IPERIA) and earlier legislation affecting improper payment and requires
extension of Departmental reporting of its data analytics performance. The intent is to ensure federal and state
entities maintain strong financial management controls to better detect, prevent, and report improper payments to the
President and the Congress in the annual Agency Financial Report (AFR).
Office of Management and Budget (OMB) Circular No. A-123, Appendix C defines an improper payment as any
payment that should not have been made or that was made in an incorrect amount under statutory, contractual,
administrative, or other legally applicable requirements. Incorrect amounts are overpayments or underpayments that
are made to eligible recipients (including inappropriate denials of payment or services, any payment that does not
account for credit for applicable discounts, payments that are for an incorrect amount, and duplicate payments). An
improper payment also includes any payment that was made to an ineligible recipient or for an ineligible good or
service, or payments for goods or services not received (except for such payments authorized by law). In addition,
when an agency’s review is unable to discern whether a payment was proper as a result of insufficient or lack of
documentation, this payment must also be considered an improper payment.
The DHA reports its improper payments and payment recapture programs in accordance with applicable laws and
regulations. The following subcategories are included in this section:
I. Risk Assessment
II. Payment Reporting
a. Root Causes
b. Corrective Actions
III. Recapture of Improper Payment Reporting
IV. Agency Improvement of Payment Accuracy with the Do Not Pay Initiative
V. Barriers
VI. Accountability
VII. Agency Information Systems and Other Infrastructure
VIII. Sampling and Estimation
IX. Significant Accomplishments
The DHA reports improper payments for the MHS TRICARE purchased health care program for payments made by
the DHA to private sector contractors for delivery of health care services to TRICARE eligible beneficiaries. For
FY 2018 the Agency reports improper payments for the following private sector contracts, DHA administrative
costs and other plans and programs:
Managed Care Support Contracts (MCSCs)
o T-3 North Region, HealthNet Federal Services
o T-3 South Region, Humana Government Business
o T-3 West Region, UnitedHealthcare Military and Veterans
TRICARE Dual Eligible Fiscal Intermediary Contract (TDEFIC)
TRICARE Overseas Program (TOP)
TRICARE Pharmacy Program (TPharm)
45
Active Duty Dental Program (ADD)
DHA Administrative Contract Cost
Other
o Uniformed Services Family Health Plan (USFHP)
o Women, Infants, and Children (WIC)
o TRICARE Dental Program
o TRICARE Retiree Dental Program
o Mail Order Pharmacy
I. Risk Assessment
The DHA risk assessment process is managed through contracts with an external independent contractor (EIC) to
provide an independent, impartial review of reimbursements and claims processing procedures used by DHA’s
purchased-care contractors. The EIC identifies improper payments resulting from the contractors’ noncompliance
with The Military Health Care System (collectively referred to as TRICARE in this report) benefit and/or
reimbursement policies, regulations, and contract requirements. The risk level of programs is evaluated based on
results of these compliance reviews.
In FY 2018, the Agency applied statistical sampling estimation methods to produce and report statistically valid
improper payment estimates for the Military Health Benefits Program. In accordance with OMB Circle A-123,
Appendix C, agencies are not required to perform additional risk assessments on programs reporting improper
payment estimates. However, any new programs identified must be assessed for improper payment risk prior to
reporting an improper payment estimate. DHA had no new program(s) implemented in FY 2017, and therefore no
additional risk assessment was required for FY 2018 reporting.
II. Payment Reporting
Table 1 reports the estimated amounts that were improperly paid and the corresponding percent by program for FY
2018. It also reports the estimated amount of improper payments that resulted in overpayments or under payments
and the DHA contractual reduction targets by program for FY 2019.
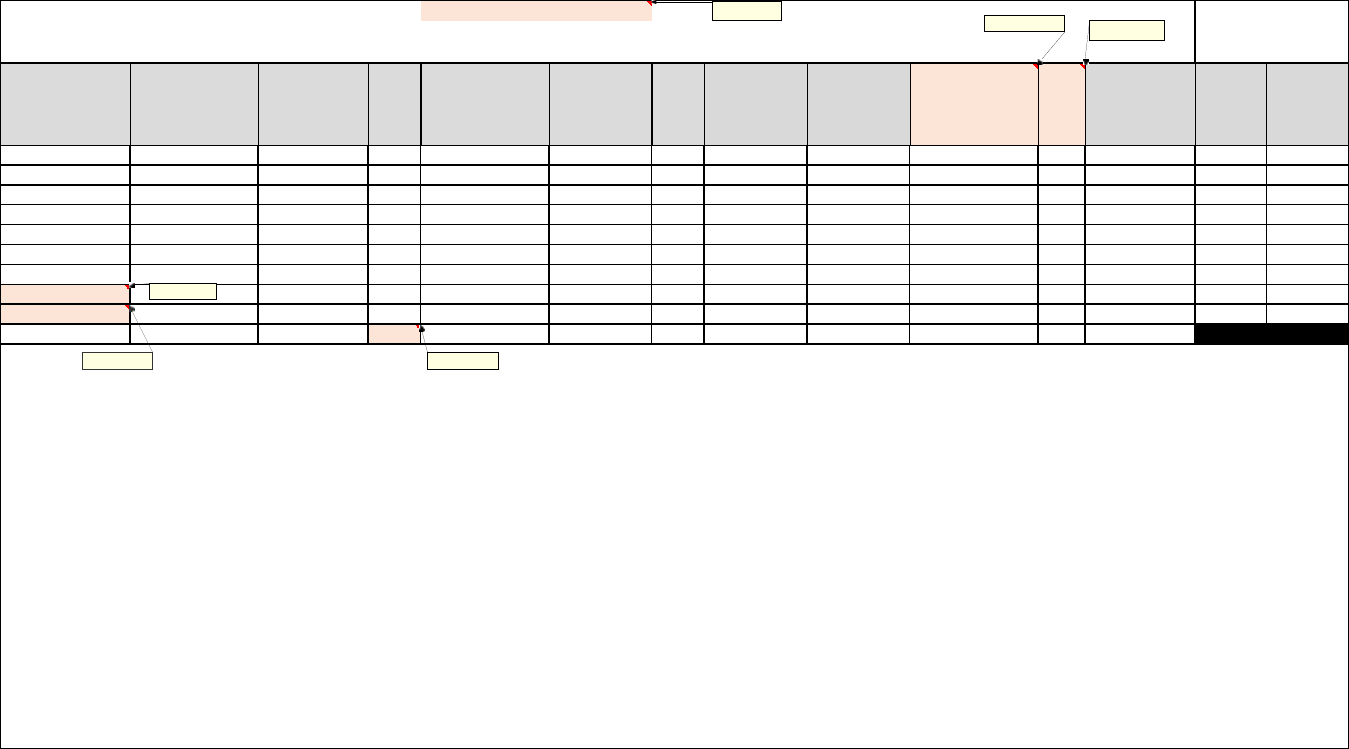
46
Program Name
FY 2017
Outlays
($M)
FY 2017
IP Amount
($M)
FY 2017
IP Rate
FY 2018
Outlays
($M)
FY 2018
IP Amount
($M)
FY 2018
IP Rate
FY2018
Over-paymen
t
$
FY2018
Under-
payment $
FY2019 Est.
Outlays
FY2019 Est.
IP %
FY2019 Est.
IP $
Month and
Year start
date for data
Month and
Year end dat
e
for data
T3 North Region
$ 3,513.32 $ 18.29 0.43% $ 3,548.47 $ 12.90 0.36% $ 6.85 $ 6.06 $ 3,686.86 0.85% $ 31.34 10/1/2016 9/30/2017
T3 South Region
$ 4,632.31 $ 18.41 0.71% $ 4,451.16 $ 29.71 0.67% $ 25.57 $ 4.14 $ 4,624.75 1.29% $ 59.66 10/1/2016 9/30/2017
T3 West Region
$ 3,985.06 $ 32.21 1.37% $ 3,668.40 $ 23.72 0.65% $ 18.34 $ 5.37 $ 3,811.46 0.93% $ 35.45 10/1/2016 9/30/2017
TDEFIC
$ 3,558.68 $ 7.60 0.38% $ 3,531.99 $ 8.48 0.24% $ 6.08 $ 2.40 $ 3,669.74 0.66% $ 24.22 10/1/2016 9/30/2017
TOP
$ 238.37 $ 2.71 1.36% $ 234.32 $ 3.36 1.43% $ 2.80 $ 0.56 $ 243.46 1.28% $ 3.12 9/1/2016 8/31/2017
TPharm
$ 3,161.13 $ 70.21 0.74% $ 2,758.49 $ 11.86 0.43% $ 11.75 $ 0.12 $ 2,866.07 1.35% $ 38.69 11/1/2016 10/31/2017
ADDP
$ 81.26 $ 0.75 0.30% $ 82.79 $ 1.21 1.46% $ 1.00 $ 0.22 $ 86.02 1.62% $ 1.39 8/1/2016 7/31/2017
DHA Administrative
$ 751.73 $ - 0.00% $ - $ - $ 781.05 0.00% $ - 10/1/2016 9/30/2017
Other
$ 4,269.21 $ - 0.00% $ - $ - $ 4,435.71 0.00% $ - 10/1/2016 9/30/2017
TOTAL
$ 23,883.30 $ 150.17 0.74% $ 23,296.55 $ 91.24 0.39% $ 72.38 $ 18.86 $ 24,205.12 0.80% $ 193.87
Footnotes:
3–DHAestablisheditsFY2019Est.IP%basedonatrendofactualimproperpaymentdatafromprioryears.ThesefiguresareestimatedtobehigherthantheFY2018actualsasaresultofDHA’simplementationofmedicalrecord
reviews(whichhavethepotentialtoidentifyadditionalimproperpayments)andtheimplementationofNDAA2017legislativerequirements,whichestablishedchangestotheTRICAREprogramthatcouldresultinincreasedpayment
errors.
4‐“DHAAdministrative”datarepresentspaymentssharedamongmultiplecontractorstoadministertheTRICAREprogram.ThesecostsincludecontractuallydefinedclaimratesforprocessingTRICAREclaims,andnon‐claimrate
administrativecosts(i.e.,contractchangeorders,permemberpermonthchargesandcontractincentivepayments).PaymentsarevalidatedviaTEDsystemprogramedits,CORreview/validationprocedures,and/orinternal/external
financialaudits.
5‐“Other”datarepresentscontractsthatarenotincludedinDHAEICindependentauditsbutwhichhaveinternalandexternalpre‐andpost‐paymentcontrols.Thefollowingcontractsareincludedinthe“Other”category:
a.UniformedServicesFamilyHealthPlan(“USFHP”)
b.Women,Infants,andChildren(“WIC”)
c.TRICAREDentalProgram(“TDP”)
d.TRICARERetireeDentalProgram(“TRDP”)
e.MailOrderPharmacy(“MOP”)
6‐The‘FY2017IPRate’of0.63%doesnotrepresentatruestatisticalestimatefortheagencybecausethe2015'10‐2016'09lowdollarTPharmauditthatwasnotconducted(duetothecontractoroptingoutofparticipatinginthe
audit,asapprovedbytheContractingOfficer).Thisauditrepresented$138,057,695paiddollars.
Improper Payment Reduction Outlook
($ in millions)
12 month Sampling
Timeframe for FY
2018 data
Table 1
2–The'FY2019Est.Outlays'werecalculatedusingtheOMBCPI‐UAnnualAveragesandPercentChangeTable.AsDHAreports12monthsinarrears,theFY2018CPI‐UmedicalpercentchangewasusedtocalculatetheFY2019
outlayestimates.
1‐DHAreportsdata12monthsinarrears,thusthisFY2018AFRincludesdatafromFY2017reviews.
Footnote 1
Footnote 3
Footnote 4
Footnote 5 Footnote 6
Footnote 2

47
Program Name
CY
Confidence
Level
CY Margin of Error
T3 North Region
90% 0.20%
T3 South Region
90% 0.25%
T3 West Region
90% 0.27%
TDEFIC
90% 0.29%
TOP
90% 0.33%
TPharm
90% 0.25%
ADDP
90% 0.56%
DHA Administrative
90% 0.00%
Other
90% 0.00%
TOTAL
90% 0.09%
Table 2
CY Estimate Statistical Information
Table A below reports the estimated amount and percentage of payments made correctly under the DHA Health
Benefits Program in FY 2017.
Table A: Amount and Percentage of DHA Improper vs. Proper Payments
Table 2 below provides current year estimate statistical information.
0.36%
$12,902,218
0.67%
$29,708,843
0.65%
$23,715,687
0.24%
$8,480,079
1.43%
$3,358,967
0.43%
$11,864,588
1.46%
$1,211,294
0.00%
$0
0.00%
$0
99.64%
$3,535,568,961
99.33%
$4,421,449,419
99.35%
$3,644,680,306
99.76%
$3,523,510,522
98.57%
$230,962,396
99.57%
$2,746,627,445
98.54%
$81,576,406
100.00%
$751,728,533
100.00%
$4,269,209,000
$0
$500,000,000
$1,000,000,000
$1,500,000,000
$2,000,000,000
$2,500,000,000
$3,000,000,000
$3,500,000,000
$4,000,000,000
$4,500,000,000
$5,000,000,000
ImproperPaymentsvsProperPaymentsbyContract
ImproperPayments ProperPayments
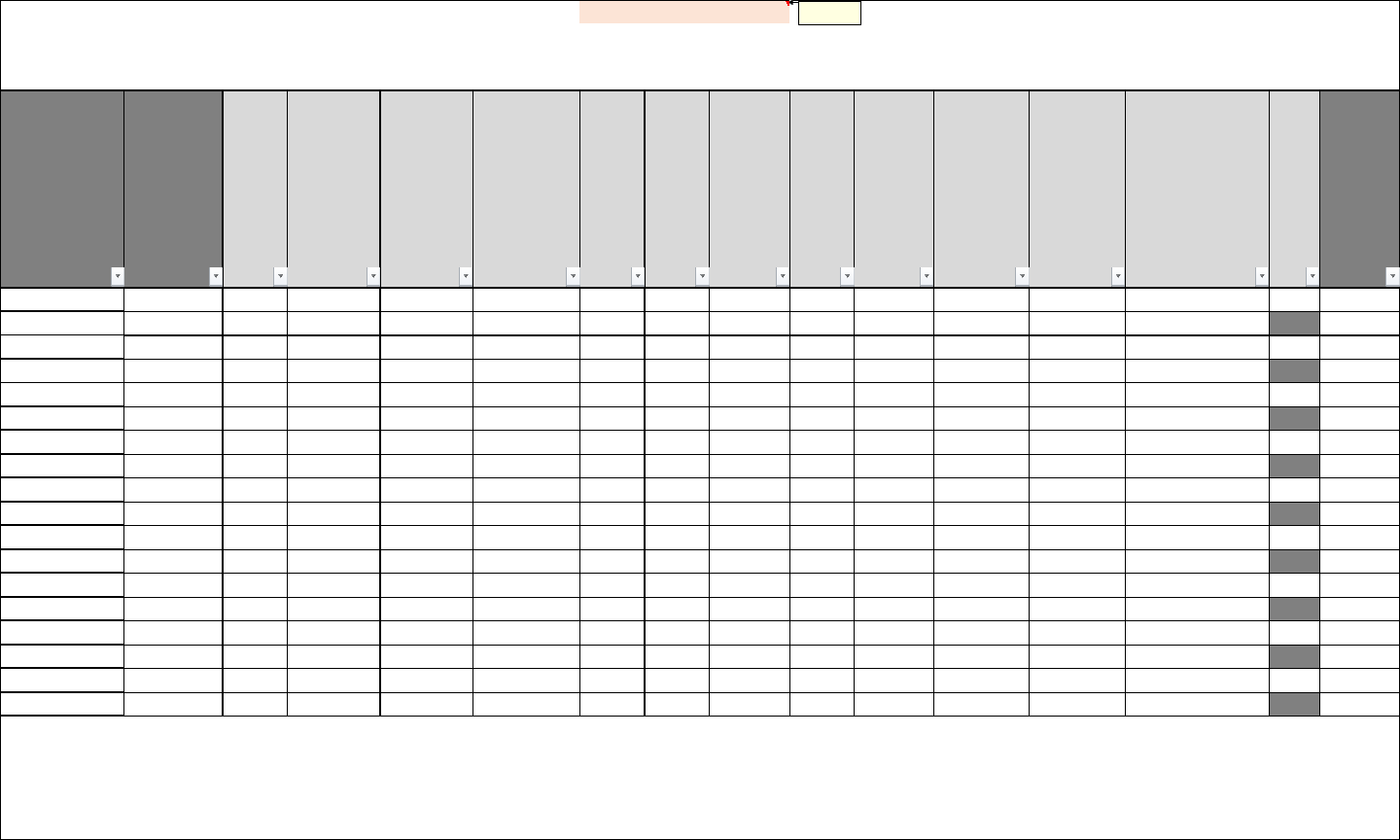
48
Table 3 reports the root cause for overpayments and underpayments by amount and by program for FY 2018.
Program Name
Payment Type
Program Design or
Structural Issue
Inability to Authenticate
Eligibility: Inability to Acces
s
Data
Inability to Authenticate
Eligibility: Data Needed Doe
s
Not Exist
Failure to Verify: Death Dat
a
Failure to Verify: Financia
l
Data
Failure to Verify: Exclude
d
Party Data
Failure to Verify: Prisoner
Data
Failure to Verify: Other
Eligibility Data (explain)
Administrative or Process
Errors Made by: Federal
Agency
Administrative or Process
Errors Made by: State or
Local Agency
Administrative or Process
Errors Made by: Other
Party (e.g., participating
lender, health care
provider, or any other
organization administerin
g
Medical Necessity
Insufficient Documentatio
n
to Determine
TOTAL
T3 North Region
Overpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 6.847 $ - $ - 6.847$
T3 North Region
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 6.055 $ - 6.055$
T3 South Region
Overpayments $ - $ 0.016 $ - $ - $ - $ - $ - $ - $ - $ 25.553 $ - $ 0.002 25.571$
T3 South Region
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 4.138 $ - 4.138$
T3 West Region
Overpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 18.341 $ - $ 0.000 18.342$
T3 West Region
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 5.374 $ - 5.374$
TDEFIC
Overpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 6.081 $ - $ - 6.081$
TDEFIC
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 2.400 $ - 2.400$
TOP
Overpayments $ - $ 0.001 $ - $ - $ - $ - $ - $ - $ - $ 2.747 $ - $ 0.055 2.802$
TOP
Underpayments $ - $ 0.001 $ - $ - $ - $ - $ - $ - $ - $ 0.556 $ - 0.557$
TPharm
Overpayments $ - $ 0.000 $ - $ - $ - $ - $ - $ - $ - $ 11.650 $ 0.086 $ 0.010 11.746$
TPharm
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 0.119 $ - 0.119$
ADDP
Overpayments $ - $ 0.006 $ - $ - $ - $ - $ - $ - $ - $ 0.749 $ 0.096 $ 0.145 0.996$
ADDP
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ 0.216 $ - 0.216$
DHA Adminis trativ e
Overpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - -$
DHA Adminis trativ e
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - -$
Other
Overpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - -$
Other
Underpayments $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - $ - -$
Footnotes:
Improper Payment Root Cause Category Matrix
($ in millions)
1‐FigureswerederivedbymultiplyingtheproportionofsampleerrordollarsforeacherrorcategorybytheextrapolatedoverpaymentorunderpaymentdollarsfromTable1.Forexample,forTPharm,'MedicalNecessity'overpaymentsfromsamplestotaled$1,143.89.Allsampleoverpaymentsfromthe
TPharmsamplestotaled$156,973.23.Therefore,thiserrorcategoryaccountedfor0.7287%oftotalsampleoverpaymentdollars($1,143.89dividedby$156,973.23).0.7287%oftheTPharm‘FY2018Over‐payment$’fromTable1($11,745,514.25)yields$85,591.51.Roundedtomillions,thisnumber
becomes$0.86(whichisshowninthistable).Thisprocesswasrepeatedforeachcellinthetable.
Table 3
Footnote 1
49
A. Root Causes
The following section provides additional information regarding the root causes of improper payments for each
program reported in Table 3 above.
The DHA contracts with an EIC to conduct quarterly, semi-annual and annual compliance reviews of previously
processed healthcare claims. EIC auditors review claims to identify improper payments, and to validate the accuracy
of the claims processing procedures utilized by TRICARE private sector contractors. Overpayment or underpayment
errors can be assessed for (but not limited to) payments in the correct amount being sent to the wrong payee,
incorrect denial of a payable claim, misapplication or calculation of a patient’s deductible or co-payment/share
liability, or payment of a non-covered service or supply. In FY 2017, EIC compliance reviews determined the root
cause for over/underpayment errors was the result of the following:
Inability to Authenticate Eligibility: DHA private sector contractors incorrectly paid or denied healthcare
claim(s) as a result of an incorrect patient eligibility determination.
Administrative or Process Errors Made by Other Party: DHA’s EIC determined throughout the course of
compliance reviews that DHA private sector contractors incorrectly processed healthcare claims by either:
o Applying an incorrect reimbursement determination or methodology when processing a
healthcare claim;
o Incorrectly calculating the Government’s liability after consideration of other health insurance
(OHI) payment(s);
o Based on a patient’s healthcare claims history, incorrectly made duplicative payments for
previously paid healthcare services or supplies;
o Miscalculated the patient’s cost-share or benefit deductible liability;
o Made a payment for services or supplies which were not a TRICARE benefit or incorrectly
denied payment for services or supplies that were a TRICARE benefit;
o Incorrectly calculated the government’s reimbursement of healthcare based on a billed
amount other than what was being reported on a healthcare claim form or itemized medical
bill; or
o Incorrectly based its reimbursement determination/methodology on an incorrect procedure
code.
Medical Necessity– the claims processor failed to follow TRICARE medical necessity review policy
requirements prior to processing and paying a healthcare claim, or failed to provide the medical necessity
review documentation needed to support or substantiate the adjudication of the claim being reviewed
during audit.
Insufficient Documentation to Determine– the EIC determined dur
ing a compliance review that the claims
documentation provided by private sector contractors was insufficient and/or did not support the
adjudication of the healthcare, as a result the EIC determined the services or procedures rendered should
not have been paid.
Other: In addition to the OMB established root cause categories listed above, DHA established a number
of individual payment error categories that further defines the rational for error assessment. For FY 2018
the EIC assessed the following individual payment errors against private sector contractors:
1) Authorization/Pre-Authorization Needed – the claims processor failed to follow TRICARE
authorization or pre-authorization requirements prior to processing a payment for a healthcare
claim, or on audit failed to provide the authorization/prior-authorization documentation
needed to support the adjudication of the healthcare claim.
2) Claims Development Required – the private sector contractor processed and paid a healthcare
claim without obtaining additional or correct information needed to support or justify the
payment of the healthcare claim, as required by TRICARE policy.
3) OHI Payment Omitted – claims documentation submitted for processing contained
information of OHI payment, however the claims processor failed to consider such
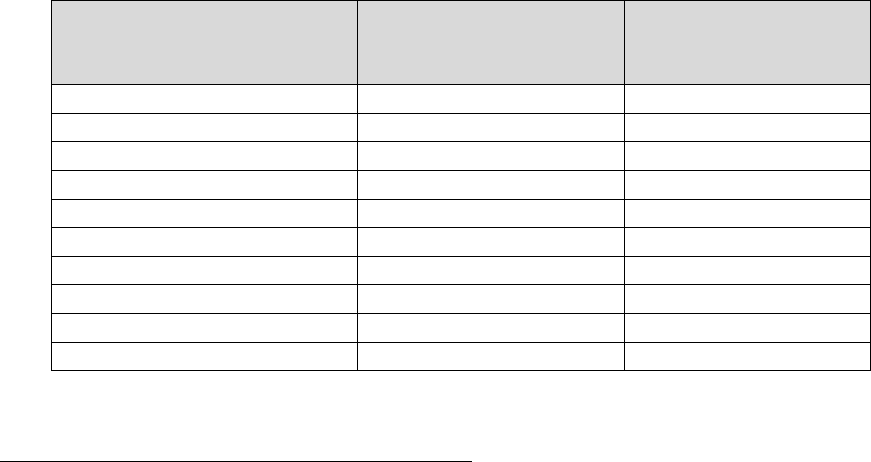
50
information when determining Government liability.
4) Diagnosis Related Group (DRG) Reimbursement Error – the claims processor made an error
in calculating the reimbursement due to an institution based on the DRG reimbursement
system.
5) Timely Filing Error – the claims processor processed and paid claims for benefit dates of
service that did not meet TRICARE timely filing requirements, and failed to obtain the
appropriate timely filing waiver(s) needed to authorize such payments.
Table 4 below reports the amount of improper payments identified in samples by contract that resulted in actual
monetary losses to the government. The purpose of this classification is to estimate the monetary loss to the Federal
Government due to improper payments. Monetary loss to the Government would be an amount that must not have
been paid and in theory should/could be recovered. This table excludes improper payments resulting from
insufficient supporting documentation.
Table 4
Improper Payment Classification
($ in millions)
Program or Activity Actual Monetary loss to
the Government
identified in Sample
Estimated Total
Monetary Loss to the
Government
T3 North Region
$ 0.19 $ 6.85
T3 South Region
$ 1.96 $ 25.57
T3 West Region
$ 1.20 $ 18.34
TDEFIC
$ 0.13 $ 6.08
TOP
$ 0.48 $ 2.80
TPharm
$ 0.16 $ 11.75
ADDP
$ 0.02 $ 1.00
DHA Administrative
$ - $ -
Other
$ - $ -
TOTAL
$ 4.14 $ 72.38
B. Corrective Actions
Military Health Benefits (FY 2018 IP Amount = $91.24M)
DHA private sector contractors are monetarily incentivized or dis-incentivized, through payment accuracy
performance standards, to reduce and/or eliminate improper payments. The fewer improper payments the
contractors make, the less money is deducted from their reimbursements. Additionally, details of the EIC
compliance reviews are shared with the private sector contractors, DHA Program Offices, private sector contract
Contracting Officers, and Contracting Officer Representatives to coordinate appropriate corrective action plans with
the respective private sector contractor. Moreover:
Upon completion of an EIC compliance review, contractors review results, formulate an action plan to
mitigate future findings, and derive a process to avoid future improper payments.
If warranted, contractor claims processing systems are modified to meet the Department’s healthcare
policy, reimbursement, or benefit requirements.
If review results show a potential error pattern for a certain type of claim, additional claims are pulled to
conduct a focused study, and adjustment actions are taken as appropriate.
51
Each private sector contractor has its own business process for evaluating compliance review results, conducting
root cause analyses to ensure the accuracy of future claims payment, and developing internal corrective action plans.
If required, DHA Contracting Officers and Contracting Officer Representatives issue contractor corrective action
plans to resolve and track noncompliance with TRICARE healthcare policy/regulations and purchased-care
contracts.
For each payment error/root cause category assessed as a result of ongoing compliance reviews, DHA will continue
to instruct private sector contractors to follow Code of Federal Regulation (CFR) Chapter 199.11 – Overpayment
Recovery instructions and to investigate and make necessary adjustments to those claims identified as having
payment errors. In addition, DHA will:
1) Modify TRICARE purchased care contracts requiring contractors to develop procedures for reporting
CAPs for each payment error category/root cause assessed against a claim during a quarterly or semi-
annual compliance review cycle as well as developing procedures for Government entities to validate
proposed CAPs;
2) Develop Contract Data Requirements List (CDRL) requirements that require contactors to provide
monthly status reports on CAPs established for each payment error category/root cause assessed for a
specified compliance review cycle (reference TRICARE Operations Manual (TOM), Chapter 14, for
additional information regarding DHA CDRL requirements);
3) Include TRICARE private sector contractor CAP reports as part of DHA’s AFR reporting to the DoD
Comptroller annually; and
4) Develop database or tracking tool to monitor TRICARE private sector contractor CAP reporting and
contractor actions taken.
III. Recapture of Improper Payments Reporting
Table 5 below reports each program or activity that exceeds $1 million or more annually that recapture payments
outside of a payment recapture audit and the amounts recovered through sources other than recapture audits.
DHA utilizes a number of different mechanisms to prevent, identify, and collect improper payments. These include
claims auditing by an EIC, contractor utilization of DHA’s Duplicate Claims System, and periodic independent
reviews of private-sector payments. This process utilizes pre and post-payment review techniques, performed
internally and by external contractors with overpayment recoveries returned to the Military Health Benefits program.
Contract payments comprise a large volume of transactions with high-dollar values; therefore, DHA is vigilant to
ensure payment accuracy. In addition to the pre and post-payment reviews, DHA also utilizes various internal
manual and automated prepayment initiatives to prevent improper payments. During FY 2017, DHA recovered
$192.26 million in overpayments as a result of overpayment errors identified by the EIC, refunds occurring in the
course of routine claims adjustments, and ongoing private sector contractor internal audits, resulting in a 266%
overpayment recovery rate.

52
Table 5
Overpayment Payment Recaptures with and without Recapture Audit Programs
($ in millions)
Overpayments Recaptured through Payment
Recapture Audits
Overpayments
Recaptured outside of
Payment Recapture
Audits
Does this
include funds
recaptured
from a High-
Priority
Program (Y/N)
Program or
Activity
Amount
Identified
in FY
2018
Amount
Recaptured
in FY 2018
Recapture
Rate in FY
2018
FY2019
Recapture
Rate
Target
Amount
Identified
in FY 2018
1
Amount
Recaptured
in FY 2018
2
N
T3 North
Region
$ 0.19 $ 3.86
N
T3 South
Region
$ 1.96 $ 5.61
N
T3 West
Region
$ 1.20 $ 7.07
N TDEFIC
$ 0.13 $ 1.92
N TOP
$ 0.48 $ 0.95
N TPharm
$ 0.16 $ 3.00
N ADDP
$ 0.02 $ 0.07
3
N
DHA
Administrative
$ - $
N Other
$ - $
TOTAL
$ 4.14 $ 22.48
Footnotes:
1 - ‘Amount Identified in FY 2018’ represents the total overpayment dollars from sampled claims.
2 - These numbers include recoupments for overpayments identified in audits as well as refunds occurring in the
course of routine claim adjustments (for claims initially paid in FY17 and other fiscal years). DHA has no way to
distinguish overpayment recoupments from routine claim adjustments."
3 - The Active Duty Dental Program (ADDP) refunds were calculated differently. The amount recovered in FY
2018 figure for ADDP represents refunds shown on contractor invoices to DHA. ADDP data is not included in the
TED system, thus contractor invoices were used because TED transactions are not available.

53
IV. Agency Improvement of Payment Accuracy with the Do Not Pay Initiative
Individual Payments. The DHA processes relatively few (5-20) case recoupment refunds each month for small
dollar amounts ($5 – $20,000). The Single Online Search service is utilized pre-payment for 100% of all case
recoupment refunds to verify (1) a business or individual has not been placed on the List of Excluded
Individuals/Entities (LEIE), and/or (2) an individual is not deceased. Any matches will be referred to the DHA
Office of General Counsel.
Vendor, Contract Payments. The DHA processes approximately 225 routine payments per month for 13 unique
contractor payees. The Single Online Search service is utilized prior to payment once a month to verify a DHA
contractor payee has not been placed on the Excluded Parties List System (EPLS) or the List of Excluded
Individuals/Entities (LEIE). Any matches are validated with the Treasury Offset Program ensuring the contractor
does not have the same Employer Identification Number (EIN) as a person’s Social Security Number (SSN). The
contractor is responsible for resolving these matching issues due to proprietary reasons. If the contractor is on the
list, the finding is referred to the assigned Contracting Officer. DHA processed approximately 312 payments
totaling $2.1 billion with no matches on the Do-Not-Pay system for Fiscal Year of 2018.
The risk for payments to a subcontractor or individual via the contractor, however, lies outside of DHA control.
DHA contractors are not required to utilize the Do-Not-Pay database, and there is no current mechanism in place to
require the contractors to use the Do-Not-Pay databases at the prepayment phase to comply with IPERA.
Table 6 below provides results of the Do Not Pay Initiative for DHA’s Military Health Benefits program.
Table 6
Results of the Do Not Pay Initiative in Preventing Improper Payments
(In millions)
Number (#)
of payments
reviewed
for possible
improper
payments
Dollars ($) of
payments
reviewed for
possible improper
payments
Number (#)
of payments
stopped
Dollars ($)
of payments
stopped
Number (#)
of potential
improper
payments
reviewed
and
determined
accurate
Dollars ($) of
potential improper
payments
reviewed and
determined
accurate
Reviews
with the
IPERIA
specified
Databases
312
$2,088,582,881.81
0
$ 0
312
$2,088,582,881.81
Reviews
with
databases
not listed in
IPERIA
0
$0
0
$ 0
0
$0
V. Barriers
The Agency did not identify any statutory or regulatory barriers limiting its corrective actions in reducing improper
payments in those programs determined in FY 2018 to be susceptible to significant improper payments.
VI. Accountability
The Under Secretary of Defense (Comptroller)/Chief Financial Officer is the Accountable Official for the

54
Department and is responsible for ensuring that, to the greatest extent possible, all DoD disbursements are accurate.
Certifying Officer Legislation, 10 U.S.C. 2773a, holds Certifying and Disbursing Officers accountable for government
funds. In accordance with this law, pecuniary liability attaches automatically when there is a fiscal irregularity, i.e., (1) a
physical loss of cash, vouchers, negotiable instruments, or supporting documents, or (2) an improper payment. This is
further captured in the DoD Financial Management Regulation (DoDFMR), Volume 5, Chapter 33, entitled “Certifying
Officers, Accountable Officials, and Review Officials.” The Department’s efforts to recover overpayments from a recipient
must be undertaken in accordance with the debt collection procedures outlined in the DoDFMR, Volume 5,Chapter 28,
“Management and Collection of Individual Debt,” and DoDFMR, Volume 10, Chapter 18, “Contractor Debt”.
The DoD FMR contains other policies that specifically address Improper Payments (DoDFMR Volume 4, Chapter
14) and Recovery Auditing (DoDFMR Volume 10, Chapter 22). Beginning in Quarter 3, FY 2013, all reporting
DoD Components were required to begin downloading their improper payment reports to the DFAS ePortal, as the
Office of the Deputy Chief Financial Officer’s Accounting & Finance Policy Directorate was designated as the
Executive Agent to manage this information and its associated reporting requirements. This centralized electronic
system allows the reporting Components to access improper payment information without regard to the time zone in
which they are located. More importantly, it allows management to ensure all Components’ submissions are timely
and accurate.
VII. Agency Information Systems and Other Infrastructure
DHA has much of the information and infrastructure needed to reduce improper payments. DHA Purchased Care
Program (managed by CRM) includes an immense volume of claims processed by TRICARE purchased care
contractors. To track programs, CRM utilizes the following systems:
TRICARE Encounter Data (TED). TED is a financial feeder system, through which all claims are
processed to OFF. TED is the entry point of claims information from DHA purchased care contractors.
TED records provide detailed information for each treatment encounter and are submitted as either an
institutional or non-institutional record. TED is primarily required by DHA to account for the expenditure
of government funds, develop statistical information, and is a data source of records for EIC audits.
Records submitted through the TED System (TEDS) must pass numerous validation edits prior to being
accepted into TEDS.
E-Commerce System (ECS). ECS is an integrated, centralized major system that improves DHA’s core
financial, contracting and business process by providing seamless integrated financial and contracting
systems.
Oracle Federal Financials (OFF). OFF is the financial subsystem of the DHA ECS. It supports budget and
accounting/financial functions and healthcare (TEDS) claims processing and contains TRICARE Claims
Management, Accounts Receivable, Accounts Payable, Purchase Orders and the General Ledger modules.
CRM uses OFF to track commitments and obligations. These transactions are submitted to DFAS and
become the primary source into financial statements.
In addition to internal DHA financial systems, DHA purchased care contractors claims processing systems are
developed and designed in accordance with TRICARE System Manual
http://manuals.tricare.osd.mil/pages/v3/DisplayManual.aspx?SeriesId=TS15 requirements and contain numerous
system edits. These edits include patient eligibility (verified via DEERS), provider eligibility, and more. If a claim
passes initial eligibility edits, benefit calculations occur based on programmed payment rules and reimbursement
methods determined by TRICARE Reimbursement Policy. The claims processing systems are able to determine the
appropriate reimbursement methodology based on information included in the healthcare claim such as type of
service, claim form type, provider specialty, etc.
Further, DHA has developed the TRICARE Duplicate Claims System (DCS). This tool facilitates the identification
of duplicate claim payments, the initiation and tracking of recoupments, required by purchased care contractors, and
the ultimate cancellation of duplicate records from the TEDS database. DHA purchased care contractors are
contractually required to use the DCS and resolve duplicate payments.
55
VIII. Sampling and Estimation
DHA followed OMB Circular A-123, Appendix C, dated October 20, 2014, when developing its sampling
methodology to select FY 2017 claims for its EIC compliance review. This statistically valid sampling methodology
met OMB’s requirements of a 90 percent confidence level and a margin of error of ±2.5 percent. By using this
methodology, DHA is able to identify valid sample sizes and project improper payment percentages for the
Agency’s improper payment program. DHA performs 100 percent pre-payment reviews of its administrative and
other program disbursements.
DHA defines samples (sets strata boundaries, calculates sample sizes, and randomly selects claims for review) and
the EIC reviews the selected claims to identify improper payments. Payment accuracy compliance reviews include
two sample types: a payment sample (to ensure payment accuracy by identifying underpayment and overpayments)
and a denied sample (to ensure appropriate claim denial). Paid samples are conducted as a stratified random sample
based on paid amounts and denied samples are conducted as a stratified random sample based on billed amounts.
Samples are drawn on either a quarterly or semi-annual basis, respective of DHA purchased care contract
requirements.
Payment Sample: Paid samples are conducted to identify improper payments and measure payment
accuracy. Depending on the private sector contract type (i.e., MCSC, TDEFIC, TOP, etc.), the universe for
a paid sample may contain between several hundred thousand to 30 million claims. All claims with
government payment amount above a high-dollar threshold (i.e., $200,000) are reviewed by the EIC.
Claims between the high-dollar threshold and a low-dollar threshold (i.e., $100) are randomly sampled
based on stratification of the government payment amount and reviewed by the EIC. Claims below the
low-dollar threshold are not included in EIC audits (but are represented by DHA Low-Dollar Internal
Reviews).
o Samples for paid claims include between 4 and 12 strata, depending on the composition of the claims
in the universe. Mathematical formulas are utilized to identify optimal strata boundary points, and
sample sizes are calculated to meet (or exceed) an estimate with a minimum of 90% confidence plus or
minus 2.5 percentage points (as stipulated in the OMB Circular A-123, Appendix C guidelines).
Low-Dollar Internal Review: In addition to the ongoing EIC quarterly and semi-annual reviews, the EIC
conducts an annual statistically valid review of low-dollar claims that fall below the low-dollar threshold
for payment samples. Audits for these EIC reviews are stratified if appropriate, given the composition of
the universe data.
Denied Sample. The primary purpose of the denied payment samples is to ensure that health care/supplies
are not being denied inappropriately (which may represent obstacles in TRICARE beneficiaries’ access to
care) by private sector contractors. Records that encompass the denied payment sample universe are
limited to records with government payment amount equal to zero. All denied claims with a billed amount
above a high-dollar threshold are reviewed, and claims below this threshold are randomly sampled based
on stratification of the billed amount. Depending on the contract type, a denied audit universe may contain
between several thousand to over 1 million claims.
o The denied payment sample is similar in design to the payment s
ample; the primary difference is that
the denied sample is stratified based on billed amount since the paid amount for a denied claim is equal
to $0.
Combining the Samples: Results from the payment sample, denied sample, and DHA’s internal low-dollar
review are all considered when DHA calculates the overall improper payment rate.
56
IX. Significant Accomplishments
The DHA is committed to full compliance with the requirements of IPERIA. As part of the Agency’s audit efforts,
DHA Components diligently review and report all payments subject to IPERIA, as well as examining processes for
identifying the complete universe of payments.
Moreover, DHA continues to explore measures to improve its internal controls to prevent improper payments, and
strengthen post payment reviews to identify and recover improper payments. To ensure the accurate and reliable
reporting of improper payments, DHA modified the TRICARE pharmacy contract to require the contractor to
participate in the annual low-dollar pharmacy claim reviews. As a result, DHA’s reported improper payment
estimates includes the complete universe of payments, as required by OMB guidance.
57
EXHIBIT 3
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
FRAUD REDUCTION REPORT
SEPTEMBER 30, 2018
OMB Circular No. A-136 requires that, “Under the Fraud Reduction and Data Analytics Act of 2015, each agency
must include in its Agency Financial Report or Performance and Accountability Reports a report on its fraud
reduction efforts undertaken in FY 2018.” The DHA OIG began working towards its goal of preventing fraud,
waste, and abuse a little over two years ago. Prior to the Deputy IG’s arrival in April 2016, the DHP Enterprise did
not have an IG – they relied on the Services and the DoD IG to provide Hotline Program and other IG services. The
DHA OIG currently has 5 government employees, 2 part-time military members, and 3 contract support personnel.
As the DHA OIG becomes fully staffed, they will operationalize the four major IG functions of Inspection,
Investigations, Teach and Train, and Assistance. The office will also evolve from a reactive to proactive model
where they spend concerted effort helping the DHP Enterprise identify and address problems through inspections
before occurrence, promoting organizational health, and enabling DHP Enterprise readiness.
The DHA OIG derives its authority to inspect and investigate from the Director, DHP Enterprise. The DHA OIG
control and reporting relationship may not be further delegated. Approval with written authority must be gained
from the Director to conduct inspections or full investigations. However, the DHA OIG can respond to requests for
assistance and can conduct informal inquiries, generally to gather initial facts to determine if a formal investigation
is warranted, without the Director’s personal approval. The DHA OIG staff are impartial and independent whose
loyalty rests with the Agency, not just with the Director.
In accordance with the authority in DoD Directive (DoDD) 5106.01, the DHA OIG maintains the DHP Enterprise
Hotline Program, ensuring that inquiries resulting from allegations are conducted in accordance with applicable
laws, DoD regulations, and policies. Per DoD Instruction (DoDI) 7050.01, the DHP Enterprise Hotline Program
provides a confidential, reliable means for individuals to report fraud, waste and abuse, violations of law, rule or
regulation, mismanagement, and classified information leaks involving the DHP Enterprise. The detection and
prevention of threats and danger to the public health and safety of the DoD and the United States are essential
elements of the Hotline mission. The DHP Enterprise Hotline maintains a public awareness campaign ensuring that
the current DoD Hotline fraud, waste, and abuse hotline poster, prepared by the DoD Office of the Inspector
General, is displayed in common work areas.
Allegations of Fraud
Hotline personnel promptly report all allegations of fraud to the appropriate Defense Criminal Investigative
Organization in accordance with DoD Instruction 5505.02, “Criminal Investigations of Fraud Offenses,” August 29,
2013, as amended. Fraud, is defined by DoD regulations as any intentional deception designed to deprive the United
States unlawfully of something of value or to secure from the United States a benefit, privilege, allowance, or
consideration to which a person or entity is not entitled. Such practices include, but are not limited to:
Offering to make a payment or accepting bribes or gratuities;
Making false statements;
Submitting false claims;
Using false weights or measures;
Evading or corrupting inspectors or other officials;
Deceiving either by suppressing the truth or misrepresenting material fact;
Adulterating or substituting materials;
Falsifying records and books of accounts;
Arranging for secret profits, kickbacks, or commissions; or
Conspiracy to do any of the above.
58
Performance Metrics and Trend Analysis
Hotline personnel collect and analyze data to:
Identify opportunities to improve the management of hotline complaints from receipt to resolution.
Identify trends that will help DHP Enterprise decision makers’ combat fraud, waste, abuse, and
mismanagement in DHP Enterprise programs and operations more effectively.
Preventing and Deterring Fraud
Curbing fraud is vital to conserving scarce health care resources and protecting beneficiaries. Fraud schemes shift
over time, but certain health care services have been consistent targets. They include services provided by durable
medical equipment (DME) suppliers, pharmacy companies, and providers. To secure the future of health care for
our beneficiaries, the DHP Enterprise must be vigilant in reducing wasteful spending and promoting better health
outcomes at lower costs. As the DHA OIG evolves and coordinates with offices to include DHP Enterprise Program
Integrity and the appropriate Defense Criminal Investigative Organization, cost savings will continue to be
recognized.
DHA OIG will ensure the workforce and culture continue to serve as a reflection of core Department values—values
that are rooted in the belief of doing the right thing.
59
DEPARTMENT OF DEFENSE
DEFENSE HEALTH AGENCY
CONTRACT RESOURCE MANAGEMENT
INDEPENDENT AUDITOR’S REPORTS

November 7, 2018
MEMORANDUM FOR UNDER SECRETARY OF DEFENSE (COMPTROLLER)/CHIEF
FINANCIAL OFFICER, DOD
ASSISTANT SECRETARY OF DEFENSE (HEALTH AFFAIRS)
DIRECTOR, DEFENSE FINANCE AND ACCOUNTING SERVICE
SUBJECT: Transmittal of the Independent Auditor’s Report on the Defense Health
Agency Contract Resource Management Financial Statements and Related
Notes for FY 2018 and FY 2017 (Project No. D2018-D000FT-0123.000,
Report No. DODIG-2019-010)
We contracted with the independent public accounting firm of Kearney & Company to
audit the Defense Health Agency–Contract Resource Management (DHA-CRM) FY 2018
and FY 2017 Financial Statements and related notes, as of September 30, 2018, and
2017, and for the years then ended, and to provide a report on internal control over
financial reporting and compliance with laws and regulations. The contract required
Kearney & Company to conduct the audit in accordance with generally accepted
government auditing standards (GAGAS); Office of Management and Budget audit
guidance; and the Government Accountability Office/President’s Council on Integrity
and Efficiency, “Financial Audit Manual,” July 2008.
1
Kearney & Company’s
Independent Auditor’s Reports are attached.
Kearney & Company’s audit resulted in an unmodified opinion. Kearney & Company
concluded that the DHA-CRM FY 2018 and FY 2017 Financial Statements and related
notes as of September 30, 2018, and 2017, and for the years then ended, are presented
fairly, in all material respects, in conformity with Generally Accepted
Accounting Principles.
1
In June 2018, the Government Accountability Office issued an updated Financial Audit Manual. Kearney & Company updated
its audit procedures to be in accordance with the updates issued in the Government Accountability Office/Council of the
Inspectors General on Integrity and Efficiency, “Financial Audit Manual,” June 2018.
INSPECTOR GENERAL
DEPARTMENT OF DEFENSE
4800 MARK CENTER DRIVE
ALEXANDRIA, VIRGINIA 22350
-
1500
60

Kearney & Company’s separate reports on “Internal Control Over Financial Reporting”
and “Compliance with Laws, Regulations, Contracts, and Grant Agreements” did not
identify any material weaknesses related to financial reporting or any instances of
noncompliance with laws, regulations, contracts, or grant agreements.
In connection with the contract, we reviewed Kearney & Company’s reports and
related documentation and discussed the audit results with Kearney & Company
representatives. Our review, as differentiated from an audit in accordance with GAGAS,
was not intended to enable us to express, and we did not express, an opinion on the
DHA-CRM FY 2018 and FY 2017 Financial Statements and related notes, conclusions
about the effectiveness of internal controls, conclusions on whether the DHA-CRM’s
financial management systems substantially complied with the “Federal Financial
Management Improvement Act of 1996,” or conclusions on whether the DHA-CRM
complied with laws and regulations.
Kearney & Company is responsible for the attached reports, dated November 7, 2018,
and the conclusions expressed in these reports. However, our review disclosed no
instances in which Kearney & Company did not comply, in all material respects,
with GAGAS.
We appreciate the courtesies extended to the staff. Please direct questions to me at
(703) 601-5945.
Lorin T. Venable, CPA
Assistant Inspector General
Financial Management and Reporting
Attachments:
As stated
61

'XNH6WUHHW6XLWH$OH[DQGULD9$
3+);ZZZNHDUQH\FRFRP
,1'(3(1'(17$8',725¶65(3257
7R
7KH$VVLVWDQW6HFUHWDU\RI'HIHQVHIRU+HDOWK$IIDLUV
7KH,QVSHFWRU*HQHUDORIWKH'HSDUWPHQWRI'HIHQVH
5HSRUWRQWKH)LQDQFLDO6WDWHPHQWV
:HKDYHDXGLWHGWKHDFFRPSDQ\LQJILQDQFLDOVWDWHPHQWVRIWKH'HIHQVH+HDOWK$JHQF\±
&RQWUDFW5HVRXUFH0DQDJHPHQW'+$&50ZKLFKFRPSULVHWKHEDODQFHVKHHWVDVRI
6HSWHPEHUDQGWKHUHODWHGVWDWHPHQWVRIQHWFRVWDQGFKDQJHVLQQHWSRVLWLRQDQG
WKHFRPELQHGVWDWHPHQWVRIEXGJHWDU\UHVRXUFHVKHUHLQDIWHUUHIHUUHGWRDVWKH³ILQDQFLDO
VWDWHPHQWV´IRUWKH\HDUVWKHQHQGHGDQGWKHUHODWHGQRWHVWRWKHILQDQFLDOVWDWHPHQWV
0DQDJHPHQW¶V5HVSRQVLELOLW\IRUWKH)LQDQFLDO6WDWHPHQWV
0DQDJHPHQWLVUHVSRQVLEOHIRUWKHSUHSDUDWLRQDQGIDLUSUHVHQWDWLRQRIWKHVHILQDQFLDOVWDWHPHQWV
LQDFFRUGDQFHZLWKDFFRXQWLQJSULQFLSOHVJHQHUDOO\DFFHSWHGLQWKH8QLWHG6WDWHVRI$PHULFDWKLV
LQFOXGHVWKHGHVLJQLPSOHPHQWDWLRQDQGPDLQWHQDQFHRILQWHUQDOFRQWUROUHOHYDQWWRWKH
SUHSDUDWLRQDQGIDLUSUHVHQWDWLRQRIILQDQFLDOVWDWHPHQWVWKDWDUHIUHHIURPPDWHULDOPLVVWDWHPHQW
ZKHWKHUGXHWRIUDXGRUHUURU
$XGLWRU¶V5HVSRQVLELOLW\
2XUUHVSRQVLELOLW\LVWRH[SUHVVDQRSLQLRQRQWKHVHILQDQFLDOVWDWHPHQWVEDVHGRQRXUDXGLWV:H
FRQGXFWHGRXUDXGLWVLQDFFRUGDQFHZLWKDXGLWLQJVWDQGDUGVJHQHUDOO\DFFHSWHGLQWKH8QLWHG
6WDWHVRI$PHULFDWKHVWDQGDUGVDSSOLFDEOHWRILQDQFLDODXGLWVFRQWDLQHGLQGovernment Auditing
StandardsLVVXHGE\WKH&RPSWUROOHU*HQHUDORIWKH8QLWHG6WDWHVDQG2IILFHRI0DQDJHPHQW
DQG%XGJHW20%%XOOHWLQ1RAudit Requirements for Federal Financial Statements
7KRVHVWDQGDUGVDQG20%%XOOHWLQ1RUHTXLUHWKDWZHSODQDQGSHUIRUPWKHDXGLWWR
REWDLQUHDVRQDEOHDVVXUDQFHDERXWZKHWKHUWKHILQDQFLDOVWDWHPHQWVDUHIUHHIURPPDWHULDO
PLVVWDWHPHQW
$QDXGLWLQYROYHVSHUIRUPLQJSURFHGXUHVWRREWDLQDXGLWHYLGHQFHDERXWWKHDPRXQWVDQG
GLVFORVXUHVLQWKHILQDQFLDOVWDWHPHQWV7KHSURFHGXUHVVHOHFWHGGHSHQGRQWKHDXGLWRU¶V
MXGJPHQWLQFOXGLQJWKHDVVHVVPHQWRIWKHULVNVRIPDWHULDOPLVVWDWHPHQWRIWKHILQDQFLDO
VWDWHPHQWVZKHWKHUGXHWRIUDXGRUHUURU,QPDNLQJWKRVHULVNDVVHVVPHQWVWKHDXGLWRU
FRQVLGHUVLQWHUQDOFRQWUROUHOHYDQWWRWKHHQWLW\¶VSUHSDUDWLRQDQGIDLUSUHVHQWDWLRQRIWKHILQDQFLDO
VWDWHPHQWVLQRUGHUWRGHVLJQDXGLWSURFHGXUHVWKDWDUHDSSURSULDWHLQWKHFLUFXPVWDQFHVEXWQRW
IRUWKHSXUSRVHRIH[SUHVVLQJDQRSLQLRQRQWKHHIIHFWLYHQHVVRIWKHHQWLW\¶VLQWHUQDOFRQWURO
$FFRUGLQJO\ZHH[SUHVVQRVXFKRSLQLRQ$QDXGLWDOVRLQFOXGHVHYDOXDWLQJWKHDSSURSULDWHQHVV
RIDFFRXQWLQJSROLFLHVXVHGDQGWKHUHDVRQDEOHQHVVRIVLJQLILFDQWDFFRXQWLQJHVWLPDWHVPDGHE\
PDQDJHPHQWDVZHOODVHYDOXDWLQJWKHRYHUDOOSUHVHQWDWLRQRIWKHILQDQFLDOVWDWHPHQWV
62

:HEHOLHYHWKDWWKHDXGLWHYLGHQFHZHKDYHREWDLQHGLVVXIILFLHQWDQGDSSURSULDWHWRSURYLGHD
EDVLVIRURXUDXGLWRSLQLRQ
2SLQLRQ
,QRXURSLQLRQWKHILQDQFLDOVWDWHPHQWVUHIHUUHGWRDERYHSUHVHQWIDLUO\LQDOOPDWHULDOUHVSHFWV
WKHILQDQFLDOSRVLWLRQRI'+$&50DVRI6HSWHPEHUDQGDQGLWVQHWFRVWRI
RSHUDWLRQVFKDQJHVLQQHWSRVLWLRQDQGEXGJHWDU\UHVRXUFHVIRUWKH\HDUVWKHQHQGHGLQ
DFFRUGDQFHZLWKDFFRXQWLQJSULQFLSOHVJHQHUDOO\DFFHSWHGLQWKH8QLWHG6WDWHVRI$PHULFD
2WKHU0DWWHUV
Required Supplementary Information
$FFRXQWLQJSULQFLSOHVJHQHUDOO\DFFHSWHGLQWKH8QLWHG6WDWHVRI$PHULFDUHTXLUHWKDW
0DQDJHPHQW¶V'LVFXVVLRQDQG$QDO\VLVKHUHLQDIWHUUHIHUUHGWRDVWKH³UHTXLUHGVXSSOHPHQWDU\
LQIRUPDWLRQ´EHSUHVHQWHGWRVXSSOHPHQWWKHILQDQFLDOVWDWHPHQWV6XFKLQIRUPDWLRQDOWKRXJK
QRWDSDUWRIWKHILQDQFLDOVWDWHPHQWVLVUHTXLUHGE\20%DQGWKH)HGHUDO$FFRXQWLQJ6WDQGDUGV
$GYLVRU\%RDUG)$6$%ZKRFRQVLGHULWWREHDQHVVHQWLDOSDUWRIILQDQFLDOUHSRUWLQJIRU
SODFLQJWKHILQDQFLDOVWDWHPHQWVLQDQDSSURSULDWHRSHUDWLRQDOHFRQRPLFRUKLVWRULFDOFRQWH[W
:HKDYHDSSOLHGFHUWDLQOLPLWHGSURFHGXUHVWRWKHUHTXLUHGVXSSOHPHQWDU\LQIRUPDWLRQLQ
DFFRUGDQFHZLWKDXGLWLQJVWDQGDUGVJHQHUDOO\DFFHSWHGLQWKH8QLWHG6WDWHVRI$PHULFDZKLFK
FRQVLVWHGRILQTXLULHVRIPDQDJHPHQWDERXWWKHPHWKRGVRISUHSDULQJWKHLQIRUPDWLRQDQG
FRPSDULQJLWIRUFRQVLVWHQF\ZLWKPDQDJHPHQW¶VUHVSRQVHVWRRXULQTXLULHVWKHILQDQFLDO
VWDWHPHQWVDQGRWKHUNQRZOHGJHZHREWDLQHGGXULQJRXUDXGLWVRIWKHILQDQFLDOVWDWHPHQWV:H
GRQRWH[SUHVVDQRSLQLRQRUSURYLGHDQ\DVVXUDQFHRQWKHLQIRUPDWLRQEHFDXVHWKHOLPLWHG
SURFHGXUHVGRQRWSURYLGHXVZLWKVXIILFLHQWHYLGHQFHWRH[SUHVVDQRSLQLRQRUSURYLGHDQ\
DVVXUDQFH
Other Information
2XUDXGLWVZHUHFRQGXFWHGIRUWKHSXUSRVHRIIRUPLQJDQRSLQLRQRQWKHILQDQFLDOVWDWHPHQWV
WDNHQDVDZKROH2WKHULQIRUPDWLRQDVQDPHGLQWKH$JHQF\)LQDQFLDO5HSRUW$)5LV
SUHVHQWHGIRUSXUSRVHVRIDGGLWLRQDODQDO\VLVDQGLVQRWDUHTXLUHGSDUWRIWKHILQDQFLDO
VWDWHPHQWV6XFKLQIRUPDWLRQKDVQRWEHHQVXEMHFWHGWRWKHDXGLWLQJSURFHGXUHVDSSOLHGLQWKH
DXGLWVRIWKHILQDQFLDOVWDWHPHQWVDFFRUGLQJO\ZHGRQRWH[SUHVVDQRSLQLRQRUSURYLGHDQ\
DVVXUDQFHRQLW
2WKHU5HSRUWLQJ5HTXLUHGE\Government Auditing Standards
,QDFFRUGDQFHZLWKGovernment Auditing StandardsDQG20%%XOOHWLQ1RZHKDYHDOVR
LVVXHGUHSRUWVGDWHG1RYHPEHURQRXUFRQVLGHUDWLRQRI'+$&50¶VLQWHUQDOFRQWURO
RYHUILQDQFLDOUHSRUWLQJDQGRQRXUWHVWVRI'+$&50¶VFRPSOLDQFHZLWKSURYLVLRQVRI
DSSOLFDEOHODZVUHJXODWLRQVFRQWUDFWVDQGJUDQWDJUHHPHQWVDVZHOODVRWKHUPDWWHUVIRUWKH
\HDUHQGHG6HSWHPEHU7KHSXUSRVHRIWKRVHUHSRUWVLVWRGHVFULEHWKHVFRSHRIRXU
63

WHVWLQJRILQWHUQDOFRQWURORYHUILQDQFLDOUHSRUWLQJDQGFRPSOLDQFHDQGWKHUHVXOWVRIWKDWWHVWLQJ
DQGQRWWRSURYLGHDQRSLQLRQRQLQWHUQDOFRQWURORYHUILQDQFLDOUHSRUWLQJRURQFRPSOLDQFHDQG
RWKHUPDWWHUV7KRVHUHSRUWVDUHDQLQWHJUDOSDUWRIDQDXGLWSHUIRUPHGLQDFFRUGDQFHZLWK
Government Auditing Standards DQG20%%XOOHWLQ1RDQGVKRXOGEHFRQVLGHUHGLQ
DVVHVVLQJWKHUHVXOWVRIRXUDXGLWV
$OH[DQGULD9LUJLQLD
1RYHPEHU
64

'XNH6WUHHW6XLWH$OH[DQGULD9$
3+);ZZZNHDUQH\FRFRP
,1'(3(1'(17$8',725¶65(325721,17(51$/&21752/29(5
),1$1&,$/5(3257,1*
7R
7KH$VVLVWDQW6HFUHWDU\RI'HIHQVHIRU+HDOWK$IIDLUV
7KH,QVSHFWRU*HQHUDORIWKH'HSDUWPHQWRI'HIHQVH
:HKDYHDXGLWHGWKHILQDQFLDOVWDWHPHQWVRIWKH'HIHQVH+HDOWK$JHQF\'+$±&RQWUDFW
5HVRXUFH0DQDJHPHQW&50DVRIDQGIRUWKH\HDUHQGHG6HSWHPEHUDQGZHKDYH
LVVXHGRXUUHSRUWWKHUHRQGDWHG1RYHPEHU:HFRQGXFWHGRXUDXGLWLQDFFRUGDQFHZLWK
DXGLWLQJVWDQGDUGVJHQHUDOO\DFFHSWHGLQWKH8QLWHG6WDWHVRI$PHULFDWKHVWDQGDUGVDSSOLFDEOH
WRILQDQFLDODXGLWVFRQWDLQHGLQGovernment Auditing StandardsLVVXHGE\WKH&RPSWUROOHU
*HQHUDORIWKH8QLWHG6WDWHVDQG2IILFHRI0DQDJHPHQWDQG%XGJHW20%%XOOHWLQ1R
Audit Requirements for Federal Financial Statements
,QWHUQDO&RQWURORYHU)LQDQFLDO5HSRUWLQJ
,QSODQQLQJDQGSHUIRUPLQJRXUDXGLWRIWKHILQDQFLDOVWDWHPHQWVZHFRQVLGHUHG'+$&50¶V
LQWHUQDOFRQWURORYHUILQDQFLDOUHSRUWLQJLQWHUQDOFRQWUROWRGHWHUPLQHWKHDXGLWSURFHGXUHVWKDW
DUHDSSURSULDWHLQWKHFLUFXPVWDQFHVIRUWKHSXUSRVHRIH[SUHVVLQJDQRSLQLRQRQWKHILQDQFLDO
VWDWHPHQWVEXWQRWIRUWKHSXUSRVHRIH[SUHVVLQJDQRSLQLRQRQWKHHIIHFWLYHQHVVRI'+$&50¶V
LQWHUQDOFRQWURO$FFRUGLQJO\ZHGRQRWH[SUHVVDQRSLQLRQRQWKHHIIHFWLYHQHVVRI'+$
&50¶VLQWHUQDOFRQWURO:HOLPLWHGRXULQWHUQDOFRQWUROWHVWLQJWRWKRVHFRQWUROVQHFHVVDU\WR
DFKLHYHWKHREMHFWLYHVGHVFULEHGLQ20%%XOOHWLQ1R:HGLGQRWWHVWDOOLQWHUQDO
FRQWUROVUHOHYDQWWRRSHUDWLQJREMHFWLYHVDVEURDGO\GHILQHGE\WKH)HGHUDO0DQDJHUV¶)LQDQFLDO
,QWHJULW\$FWRI)0),$VXFKDVWKRVHFRQWUROVUHOHYDQWWRHQVXULQJHIILFLHQWRSHUDWLRQV
$GHILFLHQF\LQLQWHUQDOFRQWUROH[LVWVZKHQWKHGHVLJQRURSHUDWLRQRIDFRQWUROGRHVQRWDOORZ
PDQDJHPHQWRUHPSOR\HHVLQWKHQRUPDOFRXUVHRISHUIRUPLQJWKHLUDVVLJQHGIXQFWLRQVWR
SUHYHQWRUGHWHFWDQGFRUUHFWPLVVWDWHPHQWVRQDWLPHO\EDVLV$PDWHULDOZHDNQHVVLVD
GHILFLHQF\RUFRPELQDWLRQRIGHILFLHQFLHVLQLQWHUQDOFRQWUROVXFKWKDWWKHUHLVDUHDVRQDEOH
SRVVLELOLW\WKDWDPDWHULDOPLVVWDWHPHQWRIWKHHQWLW\¶VILQDQFLDOVWDWHPHQWVZLOOQRWEHSUHYHQWHG
RUGHWHFWHGDQGFRUUHFWHGRQDWLPHO\EDVLV$VLJQLILFDQWGHILFLHQF\LVDGHILFLHQF\RU
FRPELQDWLRQRIGHILFLHQFLHVLQLQWHUQDOFRQWUROWKDWLVOHVVVHYHUHWKDQDPDWHULDOZHDNQHVV\HW
LPSRUWDQWHQRXJKWRPHULWDWWHQWLRQE\WKRVHFKDUJHGZLWKJRYHUQDQFH
2XUFRQVLGHUDWLRQRILQWHUQDOFRQWUROZDVIRUWKHOLPLWHGSXUSRVHGHVFULEHGLQWKHILUVWSDUDJUDSK
RIWKLVVHFWLRQDQGZDVQRWGHVLJQHGWRLGHQWLI\DOOGHILFLHQFLHVLQLQWHUQDOFRQWUROWKDWPLJKWEH
PDWHULDOZHDNQHVVHVRUVLJQLILFDQWGHILFLHQFLHVWKHUHIRUHPDWHULDOZHDNQHVVHVRUVLJQLILFDQW
GHILFLHQFLHVPD\H[LVWWKDWZHUHQRWLGHQWLILHG*LYHQWKHVHOLPLWDWLRQVGXULQJRXUDXGLWZHGLG
QRWLGHQWLI\DQ\GHILFLHQFLHVLQLQWHUQDOFRQWUROWKDWZHFRQVLGHUWREHPDWHULDOZHDNQHVVHV
+RZHYHUPDWHULDOZHDNQHVVHVPD\H[LVWWKDWKDYHQRWEHHQLGHQWLILHG
:HQRWHGFHUWDLQDGGLWLRQDOPDWWHUVLQYROYLQJLQWHUQDOFRQWURORYHUILQDQFLDOUHSRUWLQJWKDWZH
ZLOOUHSRUWWR'+$&50¶VPDQDJHPHQWLQDVHSDUDWHOHWWHU
65

3XUSRVHRIWKLV5HSRUW
7KHSXUSRVHRIWKLVUHSRUWLVVROHO\WRGHVFULEHWKHVFRSHRIRXUWHVWLQJRILQWHUQDOFRQWURODQGWKH
UHVXOWVRIWKDWWHVWLQJDQGQRWWRSURYLGHDQRSLQLRQRQWKHHIIHFWLYHQHVVRI'+$&50¶VLQWHUQDO
FRQWURO7KLVUHSRUWLVDQLQWHJUDOSDUWRIDQDXGLWSHUIRUPHGLQDFFRUGDQFHZLWKGovernment
Auditing StandardsDQG20%%XOOHWLQ1RLQFRQVLGHULQJWKHHQWLW\¶VLQWHUQDOFRQWURO
$FFRUGLQJO\WKLVFRPPXQLFDWLRQLVQRWVXLWDEOHIRUDQ\RWKHUSXUSRVH
$OH[DQGULD9LUJLQLD
1RYHPEHU
66

'XNH6WUHHW6XLWH$OH[DQGULD9$
3+);ZZZNHDUQH\FRFRP
,1'(3(1'(17$8',725¶65(325721&203/,$1&(:,7+/$:6
5(*8/$7,216&2175$&76$1'*5$17$*5((0(176
7R
7KH$VVLVWDQW6HFUHWDU\RI'HIHQVHIRU+HDOWK$IIDLUV
7KH,QVSHFWRU*HQHUDORIWKH'HSDUWPHQWRI'HIHQVH
:HKDYHDXGLWHGWKHILQDQFLDOVWDWHPHQWVRIWKH'HIHQVH+HDOWK$JHQF\'+$±&RQWUDFW
5HVRXUFH0DQDJHPHQW&50DVRIDQGIRUWKH\HDUHQGHG6HSWHPEHUDQGZHKDYH
LVVXHGRXUUHSRUWWKHUHRQGDWHG1RYHPEHU:HFRQGXFWHGRXUDXGLWLQDFFRUGDQFHZLWK
DXGLWLQJVWDQGDUGVJHQHUDOO\DFFHSWHGLQWKH8QLWHG6WDWHVRI$PHULFDWKHVWDQGDUGVDSSOLFDEOH
WRILQDQFLDODXGLWVFRQWDLQHGLQGovernment Auditing StandardsLVVXHGE\WKH&RPSWUROOHU
*HQHUDORIWKH8QLWHG6WDWHVDQG2IILFHRI0DQDJHPHQWDQG%XGJHW20%%XOOHWLQ1R
Audit Requirements for Federal Financial Statements
&RPSOLDQFHDQG2WKHU0DWWHUV
$VSDUWRIREWDLQLQJUHDVRQDEOHDVVXUDQFHDERXWZKHWKHU'+$&50¶VILQDQFLDOVWDWHPHQWVDUH
IUHHIURPPDWHULDOPLVVWDWHPHQWZHSHUIRUPHGWHVWVRILWVFRPSOLDQFHZLWKSURYLVLRQVRI
DSSOLFDEOHODZVUHJXODWLRQVFRQWUDFWVDQGJUDQWDJUHHPHQWVQRQFRPSOLDQFHZKLFKFRXOGKDYH
DGLUHFWDQGPDWHULDOHIIHFWRQWKHILQDQFLDOVWDWHPHQWVDQGSURYLVLRQVUHIHUUHGWRLQ6HFWLRQ
DRIWKH)HGHUDO)LQDQFLDO0DQDJHPHQW,PSURYHPHQW$FWRI))0,$:HOLPLWHG
RXUWHVWVRIFRPSOLDQFHWRWKHVHSURYLVLRQVDQGGLGQRWWHVWFRPSOLDQFHZLWKDOOODZVUHJXODWLRQV
FRQWUDFWVDQGJUDQWDJUHHPHQWVDSSOLFDEOHWR'+$&503URYLGLQJDQRSLQLRQRQFRPSOLDQFH
ZLWKWKRVHSURYLVLRQVZDVQRWDQREMHFWLYHRIRXUDXGLWDFFRUGLQJO\ZHGRQRWH[SUHVVVXFKDQ
RSLQLRQ7KHUHVXOWVRIRXUWHVWVGLVFORVHGQRLQVWDQFHVRIQRQFRPSOLDQFHRURWKHUPDWWHUVWKDW
DUHUHTXLUHGWREHUHSRUWHGXQGHUGovernment Auditing StandardsDQG20%%XOOHWLQ1R
7KHUHVXOWVRIRXUWHVWVRIFRPSOLDQFHZLWK))0,$GLVFORVHGQRLQVWDQFHVLQZKLFK'+$&50
ILQDQFLDOPDQDJHPHQWV\VWHPVGLGQRWFRPSO\VXEVWDQWLDOO\ZLWKWKH)HGHUDOILQDQFLDO
PDQDJHPHQWV\VWHP¶VUHTXLUHPHQWVDSSOLFDEOH)HGHUDODFFRXQWLQJVWDQGDUGVRUDSSOLFDWLRQRI
WKH8QLWHG6WDWHV6WDQGDUG*HQHUDO/HGJHUDWWKHWUDQVDFWLRQOHYHO
67

3XUSRVHRIWKLV5HSRUW
7KHSXUSRVHRIWKLVUHSRUWLVVROHO\WRGHVFULEHWKHVFRSHRIRXUWHVWLQJRIFRPSOLDQFHDQGWKH
UHVXOWVRIWKDWWHVWLQJDQGQRWWRSURYLGHDQRSLQLRQRQWKHHIIHFWLYHQHVVRI'+$&50¶V
FRPSOLDQFH7KLVUHSRUWLVDQLQWHJUDOSDUWRIDQDXGLWSHUIRUPHGLQDFFRUGDQFHZLWKGovernment
Auditing StandardsDQG20%%XOOHWLQ1RLQFRQVLGHULQJWKHHQWLW\¶VFRPSOLDQFH
$FFRUGLQJO\WKLVFRPPXQLFDWLRQLVQRWVXLWDEOHIRUDQ\RWKHUSXUSRVH
$OH[DQGULD9LUJLQLD
1RYHPEHU
68
